Key takeaways:
Central serous retinopathy, or central serous chorioretinopathy, causes vision changes that can be permanent.
Steroids — in any form — are the most common trigger for central serous retinopathy.
Treatments for central serous retinopathy include laser eye surgery and photodynamic therapy.
All medications can cause side effects. But sometimes these side effects can be surprising and unexpected. If you’re taking steroids, you’re probably well versed on the side effects it can cause. But did you know that steroids are one of the many medications that can take a toll on your vision and eye health? Here’s what to know about steroids and how they can affect your eyes.
What is central serous retinopathy?
Central serous retinopathy, or central serous chorioretinopathy, is an eye condition that causes vision changes. Central serous retinopathy develops when fluid builds up in the back part of the eye. This fluid pushes the retina away from the back of the eye, leading to a small retinal detachment.
The retina is the part of the eye that sends light signals to the brain. The brain interprets these signals so that you can see. Since detached retinas don’t work properly, central serous retinopathy leads to vision damage.
Search and compare options
Central serous retinopathy isn’t as common as other retinal diseases like diabetic retinopathy or age-related macular degeneration. But it still makes it into the top five most common retinopathies. Central serous retinopathy is more common in men between 39 and 51 years old.
Some things increase your risk for developing central serous retinopathy — like taking corticosteroids. If steroids are part of your treatment plan, here’s what you should know about central serous retinopathy.
What causes central serous retinopathy?
Researchers aren’t sure what exactly causes central serous retinopathy. They also haven’t pinpointed why some people develop the condition more than others.
But one thing is clear — many people who develop central serous retinopathy take corticosteroids as part of a medical treatment plan for different conditions. These corticosteroids include:
Oral steroids: This includes corticosteroids in pill or liquid form, like prednisone. Oral steroids can treat flares of autoimmune conditions, asthma, and COPD (chronic obstructive pulmonary disease). They’re also part of initial therapy for many other medical conditions.
Inhaled steroids: Inhaled steroids are the first-choice treatment for asthma and COPD. They’re found in medications like fluticasone / salmeterol (Advair) and fluticasone (Flovent). Nasal steroids are another type of inhaled steroid, which treat chronic rhinitis, hay fever, and seasonal allergies. Examples include mometasone (Nasonex) and fluticasone (Flonase).
Topical steroids: Topical steroids come in creams, ointments, and lotions. You may need to use topical steroids if you have eczema, psoriasis, or other skin conditions. Topical steroids also include steroid eye drops, which treat conditions like uveitis.
It’s not clear how steroids trigger central serous retinopathy. There’s no clear information on whether higher steroid doses are more likely to trigger central serous retinopathy. It’s also not clear if people who use steroids for longer periods of time are at higher risk for developing central serous retinopathy.
Diabetes and the eyes: Learn how diabetic retinopathy can affect vision.
Why you shouldn’t stare at the sun: Solar retinopathy can cause eye pain and changes in vision. Learn more about this condition here.
Our guide to cataracts: Cataracts form when proteins inside the lens of the eye break down. This is what you can do to avoid cataracts.
Other things that have been linked to a higher risk for developing central serous retinopathy include:
Phosphodiesterase 5 inhibitor medications, like Viagra and Cialis
Autoimmune conditions, like lupus
Obstructive sleep apnea
Pregnancy
High blood pressure
What are the symptoms of central serous retinopathy?
Symptoms of central serous retinopathy include:
Blurry vision
Dark spots in the middle of your vision (scotomas)
Vision distortion that makes straight lines look wavy
Objects looking smaller than they really are (micropsia)
Decreased color perception that makes colors look less vivid or washed out
Less contrast sensitivity that makes it harder to see shades of color or gray
Read more like this
Explore these related articles, suggested for readers like you.
Always get immediate medical care if you experience new vision changes. They can be a sign of a serious eye problem. This is especially true if you need to take steroids as part of your treatment plan.
Does central serous retinopathy cause blindness?
Central serous retinopathy doesn’t usually lead to complete vision loss. Some people develop long-term vision problems, including low vision.
Others develop a hyperopic shift because of how the fluid buildup affects the back of the eye. If you have a hyperopic shift, you’ll notice that your glasses or contact prescription doesn’t seem to work anymore. You may need to adjust your prescription.
How do you diagnose central serous retinopathy?
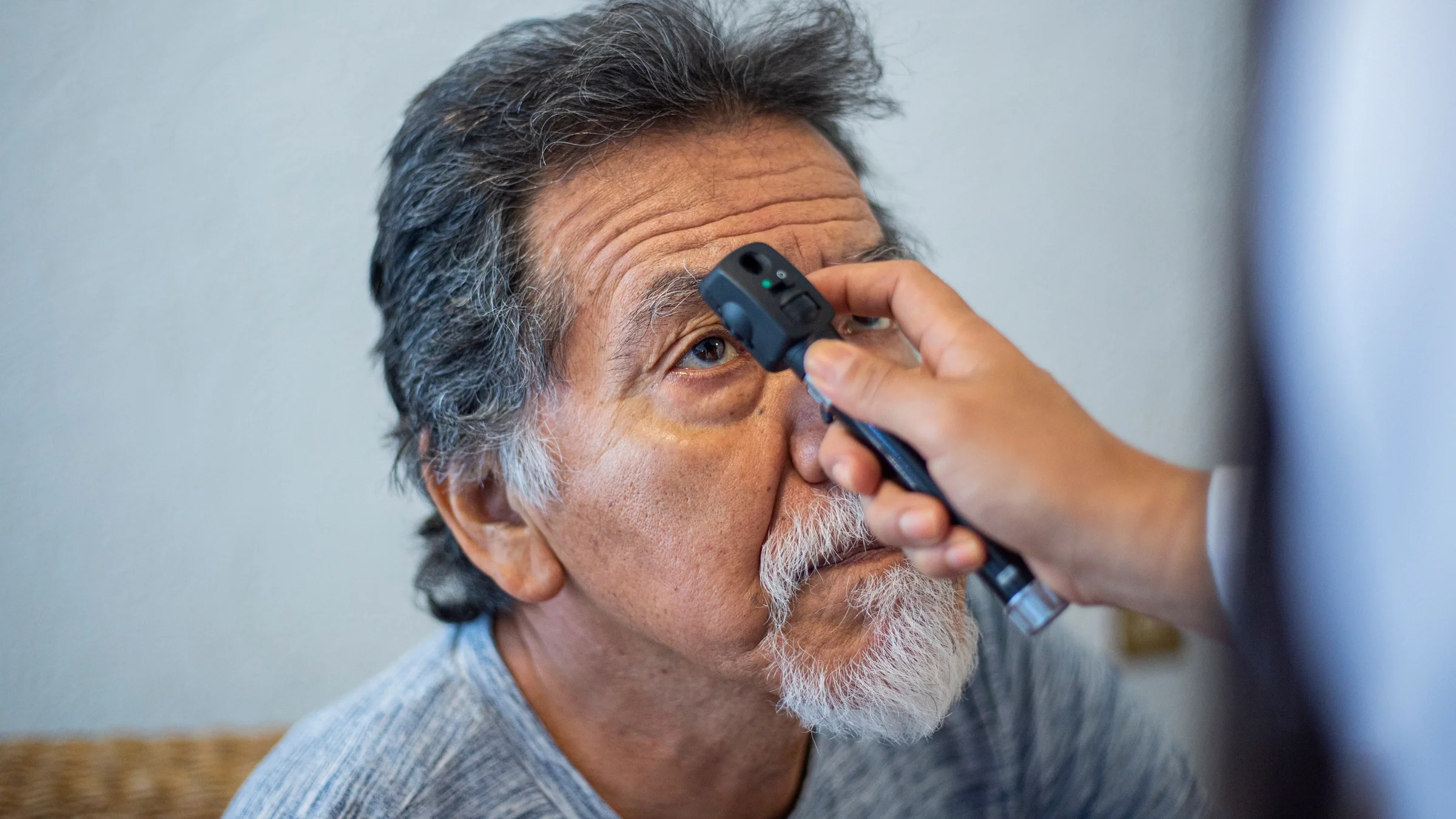
Your eye doctor can diagnose central serous retinopathy with a dilated eye exam. They’ll use a bright light and magnifying lens to look at the retina.
They might also take photographs of your retina with an optical coherence tomography (OCT). This machine allows you and your doctor to monitor the health of your retina over time. It can also help figure out if you’re responding well to treatment. You may need to do these pictures every few months or every time you have a doctor’s visit. An OCT isn’t painful.
You may also need a fluorescein angiography test. In this test, the ophthalmology team injects fluorescein dye into your arm through an IV (intravenous) line while a special machine takes photos of blood vessels in your eye. This gives important information about the health of these vessels, which can be hard to see with just a dilated eye exam.
How do you treat central serous retinopathy?
Sometimes central serous retinopathy clears up on its own within a few weeks or months.
Your eye doctor will monitor the back of your eyes closely to see if you’re getting better without treatment. If your eyes aren’t healing on their own, you may need treatment like laser eye surgery or photodynamic therapy.
These treatments seal off structures in the back of the eye so they don’t leak fluid. But they don’t always work for everyone.
Researchers are investigating other treatments for central serous retinopathy, such as:
Anti-vascular endothelial growth factor (anti-VEGF) medications work by slowing the growth of abnormal blood vessels in the eye. They are administered by injection into the eye, called intra-vitreal injection.
Mineralocorticoid receptor antagonists like spironolactone and eplerenone work by blocking a hormone that causes the body to hold on to sodium and water. Initial studies have shown that these medications may help treat central serous retinopathy.
You may also need to stop taking your corticosteroid medication. This can be a difficult decision, since your steroid therapy is likely very important to keep you healthy. You’ll need to talk to all the members of your care team to decide if this is the best option for you.
Keep in mind that you shouldn’t suddenly stop taking steroids because this can lead to serious side effects. You’ll need to stop taking them slowly, especially if you’ve been taking them for a long time. Your healthcare team can come up with a taper schedule for you to safely stop taking steroids.
What happens if you don’t treat central serous retinopathy?
Sometimes central serous retinopathy clears up on its own. But if it doesn’t, and you don’t get treatment, your vision can be permanently affected. Low vision can make it hard to do things like read, type, drive, and recognize faces or objects.
Besides central serous retinopathy, steroids can also lead to glaucoma and cataracts. So if you notice vision changes, see your eye doctor right away. You can also be proactive and get an eye exam each year to make sure your eyes stay healthy.
Frequently asked questions
Yes, taking corticosteroids can increase the risk of developing cataracts. Both oral and inhaled corticosteroid use can increase the risk of developing cataracts. Very strong topical steroids, like creams and lotions, may increase the risk of cataracts if you need to use them for a long time.
Yes, it’s safe to travel by plane if you have central serous retinopathy. Change in atmospheric pressure will not make this condition worse.
Central serous retinopathy can be considered a disability if it permanently affects your vision. Severe retinopathy that leads to permanent low vision will qualify as a disability. But some cases of central serous retinopathy resolve with time, and people’s vision goes back to normal.
Yes, taking corticosteroids can increase the risk of developing cataracts. Both oral and inhaled corticosteroid use can increase the risk of developing cataracts. Very strong topical steroids, like creams and lotions, may increase the risk of cataracts if you need to use them for a long time.
Yes, it’s safe to travel by plane if you have central serous retinopathy. Change in atmospheric pressure will not make this condition worse.
Central serous retinopathy can be considered a disability if it permanently affects your vision. Severe retinopathy that leads to permanent low vision will qualify as a disability. But some cases of central serous retinopathy resolve with time, and people’s vision goes back to normal.
The bottom line
Central serous retinopathy is an eye condition that can affect your vision. It’s caused by a fluid buildup in the back of the eye. It’s not clear why some people develop central serous retinopathy.
People who take steroids, including inhaled or topical steroids, are at higher risk for developing central serous retinopathy. If you take steroids and notice vision changes, see an eye doctor right away. You may need treatment for central serous retinopathy.

Why trust our experts?



References
Bhavsar, A. R. (2015). Can I fly with central serous retinopathy? American Academy of Ophthalmology.
Cumming, R. G., et al. (1997). Use of inhaled corticosteroids and the risk of cataracts. The New England Journal of Medicine.
Gabros, S., et al. (2025). Topical corticosteroids. StatPearls.
Haimovici, R., et al. (2003). Endocrine abnormalities in patients with central serous chorioretinopathy. Ophthalmology.
Laudate, T. M., et al. (2011). Micropsia. Encyclopedia of Clinical Neuropsychology.
Mi, C. W., et al. (2024). Central serous chorioretinopathy. American Academy of Ophthalmology.
Mukit, F. A., et al. (2025). Ocular manifestations of corticosteroids. American Academy of Ophthalmology.
Park, J. B., et al. (2022). Central serous chorioretinopathy: Treatment. Taiwan Journal of Ophthalmology.
Porter, D. (2021). What is fluorescein angiography?. American Academy of Ophthalmology.
Porter, D. (2024). What is central serous chorioretinopathy? American Academy of Ophthalmology.
Sartini, F., et al. (2019). Non-resolving, recurrent and chronic central serous chorioretinopathy: Available treatment options. Eye.
ScienceDirect. (n.d.). Metamorphopsia.
Semeraro, F., et al. (2019). Central serous chorioretinopathy: Pathogenesis and management. Clinical Ophthalmology.
Social Security Administration. (2025). If you’re blind or have low vision — how we can help.
Turbert, D. (2023). Anti-VEGF treatments. American Academy of Ophthalmology.
Turbert, D. (2024). What is optical coherence tomography? American Academy of Ophthalmology.