
Allergy Medicine: Comparing the Best OTC Allergy Medications
Key takeaways:
Allergy medicines, such as intranasal steroids, are the first-choice treatment for people with persistent allergy symptoms — but some of them take time to work.
Consider several factors when selecting an allergy medication, including your symptoms, how quickly you need relief, and side effects.
Antihistamines, a popular class of allergy medicines, can cause drowsiness. But some have less sedating effects.
There are ways to save on your allergy medications. Many options are available over the counter and as lower-cost generics. GoodRx can help make your medication more affordable.
Access savings on related medications
Table of contents

Sneezing, runny nose, and itchy eyes — these are all telltale signs of allergies. And whether you have them seasonally or year round, they can make you feel pretty miserable. Allergy medicine can help keep your symptoms in check.
But with so many choices, there’s a chance you could be taking the wrong one and not getting enough allergy relief. Here are some questions to consider before popping more allergy pills. This way, you can find one that best meets your needs.
What are the best allergy medicines to take?
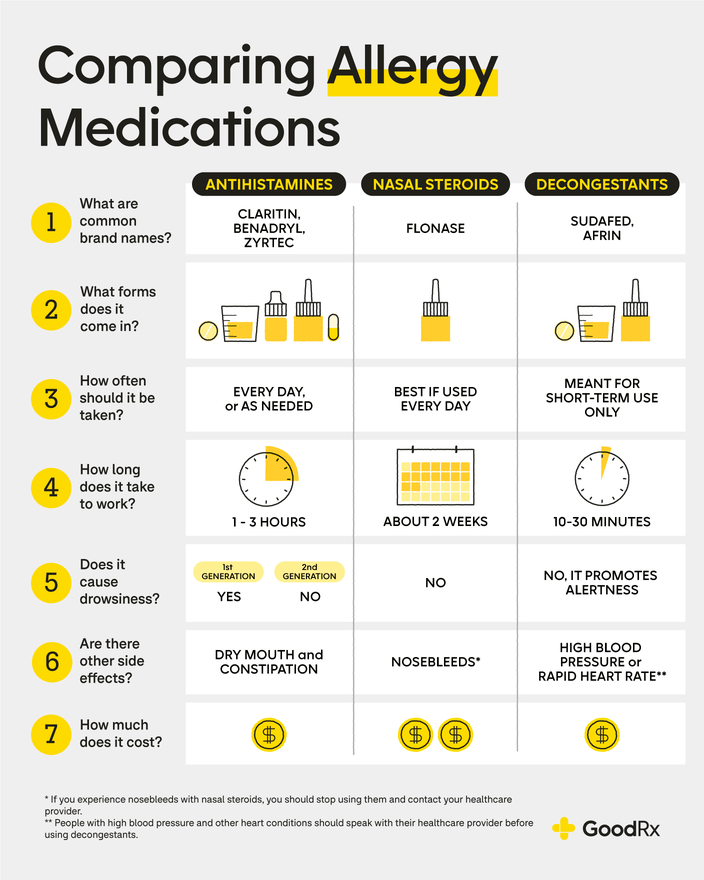
Depending on how long your allergy symptoms last, certain allergy medicines will likely work better than others. Here are the four most common kinds of allergy medicines people use.
Promotion Disclosure: GoodRx provides visitors with access to select third party offers. The placement of these offers is managed independently from our editorial coverage. GoodRx may receive compensation if you engage with an offer, but making an offer available does not influence the content our editorial staff provides. At GoodRx Health, providing accurate and trusted information and resources is our first priority. Article and video content is written and reviewed by our editorial staff with medical, healthcare policy and pricing experience. GoodRx does not endorse or recommend any product or service in connection with providing access to an offer.
Antihistamines
If your allergies only appear sporadically — say, when the pollen count is high, or you have that random encounter with your friend’s cat — oral antihistamines may be your best bet. Many of these are readily available over the counter (OTC). And they typically start working within a few hours of your first dose.
Stay healthy with CVS
Shop the brands you trust at CVS. Whether it’s wellness or beauty, get what you need at great prices.

Examples of oral OTC antihistamines include:
Benadryl (diphenhydramine)
Claritin (loratadine)
Allegra (fexofenadine)
Zyrtec (cetirizine)
Xyzal (levocetirizine)
There’s also an OTC antihistamine nasal spray available: Astepro (azelastine). It works much faster than oral antihistamines — within 15 to 30 minutes. And some studies have found that intranasal antihistamines may work better than antihistamine pills for nasal allergy symptoms, such as congestion.
Is there a “strongest” oral antihistamine? Not really. However, a review of multiple studies suggests Allegra may work better for eye-related symptoms and Xyzal may help with sneezing and nasal itching more than others. Claritin seems to be slightly less effective overall.
Histamine is a chemical our immune system releases when we come into contact with something we’re allergic to. It then triggers allergy symptoms, like a runny nose or itchy eyes. Antihistamines work by blocking areas of your body where histamine would normally attach to cause these symptoms.
While some people take antihistamines as needed for allergy symptoms, daily use is currently expert-recommended and may be an option for people looking to prevent symptoms.
Your over-the-counter (OTC) treatment guide: Dive deeper into the best OTC options for managing allergy symptoms, from decongestants to nasal sprays and more.
Alternative treatments: Some natural supplements may also help treat allergy symptoms. Learn what the experts have to say about which supplements are worth a try.
More than medication: Three people share the daily lifestyle changes that have proven effective at reducing their allergy symptoms.
In the case of seasonal allergies, you can take antihistamines before you’re exposed to an allergy trigger — like pollen. Starting the medication at least 2 weeks before allergy season typically begins can help you get the best results. This can be particularly helpful if you have frequent seasonal allergy symptoms.
Nasal steroids
If you experience daily or year-round allergies, you’ll want to look into nasal steroids. They can also be helpful if you know your seasonal allergy symptoms tend to last for several weeks or months. Experts recommend trying nasal steroids before other allergy medicines, as they tend to be the most effective option.
OTC nasal steroids include:
Similar to antihistamines, there’s no “strongest” nasal steroid. However, a review of multiple studies suggests Nasonex may be the most effective for seasonal allergies. The same review found Rhinocort to be the most effective for year-round allergies.
Nasal steroids generally take longer to work than antihistamines. But healthcare professionals consider them to be the most effective for keeping nasal allergy symptoms in check over time. As a group, they may also be more effective at preventing nasal congestion compared to oral antihistamines.
Here’s how they’re thought to work: When you have allergies, a complicated series of reactions occur in your immune system between the moment you sense an allergen and when you get that runny nose. Nasal steroids act early on in these reactions — even before histamine is made — and prevent the processes that lead to a full-blown allergic response.
Decongestants
Decongestants help improve symptoms by relieving nasal and sinus congestion. They typically work quicker than other allergy medicines. This makes them an attractive option for fast relief.
Decongestants available without a prescription include:
Sudafed (pseudoephedrine) — kept behind the pharmacy counter
Afrin (oxymetazoline)
Neo-Synephrine (phenylephrine nasal spray)
Some allergy medicines, such as Allegra-D (fexofenadine / pseudoephedrine) and Claritin-D (loratadine / pseudoephedrine), combine both decongestants and antihistamines into the same pill so that they can target congestion and other allergy symptoms at the same time.
Decongestants can help you breathe a little easier if you’re stuffed up, but they shouldn’t be taken long term. Also, it’s important to know that nasal decongestant sprays, like Afrin, can make your congestion worse if they’re used for more than a few days (called rebound congestion). So it’s best to use them sparingly.
Oral decongestants, like Sudafed, also shouldn’t be taken if you have certain heart conditions, including high blood pressure. If you have these health conditions, talk to a pharmacist or other healthcare professional first before giving them a try.
Mast cell stabilizers
Mast cell stabilizers are another allergy medicine option. But they’re not a good option for quick relief, as they take longer to start working. NasalCrom (cromolyn sodium nasal spray) is the only OTC nasal mast cell stabilizer currently available.
Mast cell stabilizers work by preventing certain cells (called mast cells) from releasing histamine. They’re generally less effective than other allergy medicines, especially for seasonal allergies. But they could be an option if you have year-round allergies. And they’re considered one of the safest allergy medicines to use during pregnancy.
What is the best allergy medicine?
The short answer is — it depends. There are a few things to consider when selecting the right allergy medicine for you:
How quickly you need relief
Your symptoms
Side effects
Cost
Fast-acting medications, like decongestants and antihistamines, work quickly if you’re experiencing symptoms. But while antihistamines can be taken daily, decongestants should only be taken as needed in the short term.
Antihistamines and nasal steroids can be good options for preventing symptoms if taken daily before allergy season hits. Experts currently recommend nasal steroids as the first-choice treatment for people with persistent symptoms. If your symptoms only happen every now and then, an oral or intranasal antihistamine would be a good first choice.
Keep in mind that not all antihistamines are created equal — certain ones have a higher risk of drowsiness. But all antihistamines can potentially make you sleepy. So it’s best to see how you respond to them before engaging in activities that require alertness or concentration.
How long will it take for your allergy medicine to work?
When you’re experiencing allergy symptoms, you want to feel better — and fast. But each product works differently and treats specific symptoms. So you should select the allergy medicine that will help you the most.
Decongestants: These offer the fastest relief. Nasal spray options should work within about 10 minutes, and oral options work within 30 to 60 minutes.
Oral antihistamines: These are another quick-relief option. Many work within about 1 to 2 hours.
Nasal antihistamine sprays: These also start working fast, about 15 to 30 minutes after using them.
Nasal steroids: These take longer to start working — a few days to 2 weeks for full effects.
Mast cell stabilizers: These take the longest to work, about 2 to 6 weeks.
Will your allergy medicine make you drowsy?
Like all medications, allergy medicines can have side effects. This can include drowsiness, depending on which type of medication you take. We’ve broken down the potential side effects that different allergy medicines can cause below.
Nasal steroids side effects
Nasal steroids don’t typically cause drowsiness. Serious side effects with nasal steroid sprays are rare because the body absorbs very little of these medicines. They do, however, carry the risk of nasal tissue inflammation. That’s why it’s important to have regular checkups with your primary care provider when using these medications for long periods of time.
Decongestants side effects
Decongestants aren’t associated with drowsiness. In fact, they can even keep you awake if you take them too close to bedtime. Other common side effects of oral decongestants include headache, anxiety, and raised heart rate or blood pressure.
First-generation antihistamines side effects
Drowsiness is a common side effect of older, first-generation antihistamines like Benadryl. These medications work quickly to control allergy symptoms. But they can pass into your brain and cause drowsiness along with other neurological symptoms, like dizziness.
Second-generation antihistamines side effects
Drowsiness and other brain-related side effects are less of an issue with newer, second-generation antihistamines, such as Claritin. This is because they’re less likely to enter the brain.
Zyrtec, however, is an exception — while it is a second-generation antihistamine, you may be more likely to get sleepy from taking it compared to Claritin or Allegra.
Possible side effects of second-generation antihistamines include:
Dry mouth
Headache
Dizziness
Ringing in the ear (tinnitus)
Take our quiz: Allergy medications
Prescription vs. OTC allergy medicines
Many allergy medicines are available OTC. But there are some that you need a prescription to purchase. These are some examples of prescription allergy medicines:
Clarinex (desloratadine) — an oral antihistamine
Vistaril (hydroxyzine) — an oral antihistamine
Patanase (olopatadine) — a nasal antihistamine spray
Flunisolide — a nasal steroid
Qnasl (Beclomethasone) — a nasal steroid
Omnaris (ciclesonide) — a nasal steroid
Prescription allergy medicines aren’t necessarily better than OTC options. Experts generally don’t recommend specific medications within a class for allergy symptoms.
However, some prescription-only medications have other uses besides allergies. For instance, Vistaril can be prescribed for itching or anxiety. And Qnasl can help prevent nasal polyps after surgery. So, if you have allergies and certain non-allergy symptoms, your prescriber may recommend a medication that can treat both.
How to save on your allergy medicine
There are many ways to save on your allergy medicine. GoodRx can help you navigate your options. You can find allergy medications for as low as $5 with a free GoodRx coupon. And if a healthcare professional writes you a prescription for an OTC allergy medicine, you can apply a GoodRx coupon to it.
The table below lists some common OTC allergy medicines and how much you might save if you use GoodRx.
Medication name | Type of allergy medicine | Savings with GoodRx |
|---|---|---|
Allegra (fexofenadine) | Oral antihistamine | As low as $7.66 for the generic version |
Benadryl (diphenhydramine) | Oral antihistamine | As low as $1.20 for the generic version |
Claritin (loratadine) | Oral antihistamine | As low as $5.95 for the generic version |
Xyzal (levocetirizine) | Oral antihistamine | As low as $9.00 for the generic version |
Zyrtec (cetirizine) | Oral antihistamine | As low as $3.16 for the generic version |
Astepro (azelastine) | Nasal antihistamine spray | As low as $17.54 for the generic version |
Flonase (fluticasone propionate) | Nasal steroid | As low as $16.60 for the generic version |
Nasacort (triamcinolone) | Nasal steroid | As low as $10.69 for the generic version |
Nasonex (mometasone) | Nasal steroid | As low as $40.33 for the generic version |
Rhinocort (budesonide) | Nasal steroid | As low as $10.16 for the generic version |
Afrin (oxymetazoline) | Nasal decongestant spray | As low as $4.73 for the generic version |
Neo-Synephrine (phenylephrine) | Nasal decongestant spray | As low as $4.56 for the generic version |
Nasalcrom (cromolyn sodium) | Mast cell stabilizer | As low as $6.89 for the generic version |
Frequently asked questions
Experts typically recommend nasal steroids, such as Flonase, for persistent or severe allergies. Oral or nasal antihistamines can be a good option if your symptoms only happen from time to time.
Most people can safely take oral antihistamine pills every day. Popular oral OTC antihistamines include Claritin, Zyrtec, and Benadryl. But not all allergy pills are safe to take long term. Avoid taking oral decongestants, such as Sudafed, for longer than 7 days in a row. Long-term use can raise your risk of side effects, such as raised blood pressure or heart rate.
Experts don’t recommend Claritin or Zyrtec over the other for seasonal allergies. Both work similarly well for treating most allergy symptoms. But some studies suggest Claritin may be slightly less effective than other oral antihistamines for some people. However, Zyrtec is more likely to cause drowsiness than Claritin.
The bottom line
There are many allergy medicines available. Decongestants, such as Sudafed (pseudoephedrine), provide the fastest relief but shouldn’t be taken long term. Antihistamines, such as Claritin (loratadine), can provide quick relief and can help prevent symptoms if taken every day. Nasal steroids, such as Flonase (fluticasone propionate), are among the most effective allergy medicines but can take up to 2 weeks to fully work.
Talk to your primary care provider or pharmacist about which allergy medicine would be the best option for you. They can help ensure that you take them properly for the best results.
Why trust our experts?


References
Derendorf, H., et al. (2008). Molecular and clinical pharmacology of intranasal corticosteroids: Clinical and therapeutic implications. Allergy.
Emeryk, A., et al. (2019). New guidelines for the treatment of seasonal allergic rhinitis. Advances in Dermatology and Allergology.
FamilyDoctor.org. (2023). Decongestants: OTC relief for congestion.
Farzam, K., et al. (2023). Antihistamines. StatPearls.
Greisner, W. A., 3rd. (2004). Onset of action for the relief of allergic rhinitis symptoms with second-generation antihistamines. Allergy and Asthma Proceedings.
Hong, D., et al. (2023). Efficacy of different oral H1 antihistamine treatments on allergic rhinitis: A systematic review and network meta-analysis of randomized controlled trials. Brazilian Journal of Otorhinolaryngology.
Mann, R. D., et al. (2000). Sedation with ‘non-sedating’ antihistamines: Four prescription-event monitoring studies in general practice. British Medical Journal.
MedlinePlus. (2021). Nasal corticosteroid sprays.
Minutello, K., et al. (2024). Cromolyn sodium. StatPearls.
Patel, R. H., et al. (2023). Biochemistry, histamine. StatPearls.
Scadding, G. K., et al. (2017). BSACI guideline for the diagnosis and management of allergic and non-allergic rhinitis (revised edition 2017; first edition 2007). Clinical and Experimental Allergy.
Seidman, M. D., et al. (2015). Clinical practice guideline: Allergic rhinitis. Otolaryngology-Head and Neck Surgery.
Soe, K. K., et al. (2023). Comparative efficacy and acceptability of licensed dose intranasal corticosteroids for moderate-to-severe allergic rhinitis: A systematic review and network meta-analysis. Frontiers in Pharmacology.
Sur, D. K. C., et al. (2015). Treatment of allergic rhinitis. American Family Physician.

























