Key takeaways:
Brian Gregg has been hospitalized six times with pneumonia, a severe respiratory infection.
During his most recent bout, he remembers feeling extreme fatigue. He also had muscle pain, fever, headache, chills, and difficulty breathing.
Hospitalization for pneumonia can be physically and emotionally draining.
I’ve been hospitalized six times with pneumonia. I have no idea why I might be more vulnerable than others. My lungs are otherwise healthy.
But when it comes to pneumonia — a severe respiratory infection — I’m a bit of an unfortunate expert.
In a 6-year span from fifth grade to ninth grade, I spent time in the hospital every other year with it. If that wasn’t bad enough, pneumonia can also cause you to throw up, as I learned the hard way. I remember puking in the school hallway in seventh grade, and in ninth grade, I didn’t even make it out of my seat before vomiting in algebra class. Those traumatic experiences stick with you, even 40 years later.
Other pneumonia symptoms can include fever, cough, chest pain, shortness of breath, fatigue, and nausea.
My most vivid memories of those hospital stays are the ’70s/’80s-era penicillin shots. The needles went in deeper and stayed in longer than any shot I’ve received since. I constantly blew into an earlier version of the incentive spirometer. I hoped to raise the little ball high enough for the doctor to judge whether my damaged lungs were healthy enough for me to go home.
In college, I made the mistake of going to the university’s healthcare center for pneumonia. A doctor-in-training decided to treat my 105-degree temperature with an ice bath. That night still ranks as one of the most unpleasant of my life. It was followed by an extended stay in the local hospital, where the professionals took over.
Next was a rather unmemorable and short hospital stay during one of my first few years out of college. I lived in a town 8 hours from my family and dealt with the treatment and recovery alone.
My last and most recent bout with pneumonia, in 2017 at the age of 50, is the most unforgettable.
What pneumonia feels like
My latest stint with pneumonia began when my wife and I tackled a great deal of yard work one spring Sunday. We started by power washing our patio and then spread 10 yards of mulch around our yard. For 10 hours, we used shovels, a pitchfork, and a wheelbarrow to haul the mulch around our third-of-an-acre lot.
Pneumonia is caused by a bacteria, virus, or fungus, and I’m convinced we stirred something up that day. We didn’t wear masks.


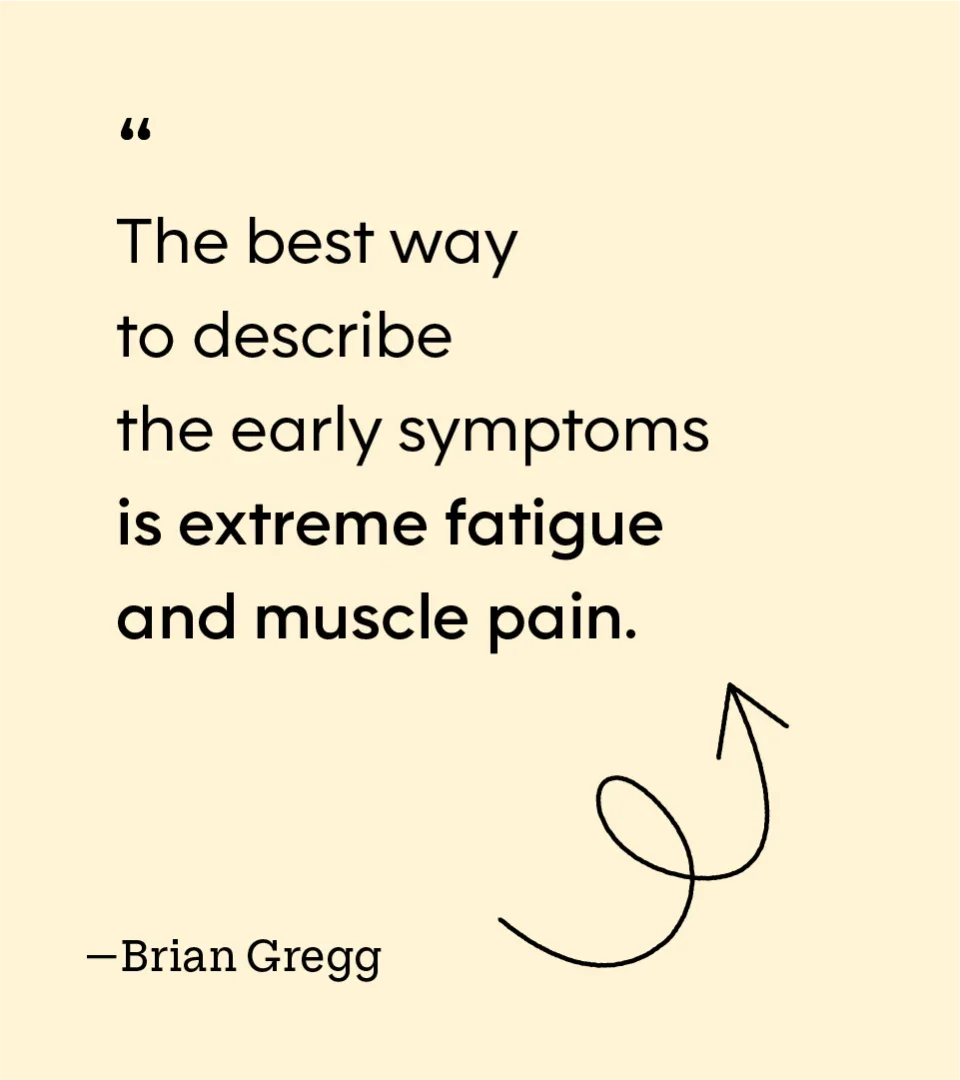
By Wednesday, we both were sick. I came home early from work, sat in a chair, and didn’t move for hours. My wife did the same in a chair across from me. The best way to describe the early symptoms is extreme fatigue and muscle pain. It was hard to drink water, so I was getting more dehydrated by the minute.
I felt like I didn’t have the strength to get out of that chair. Still, we had two children to care for, so we did as little as possible to get by that night, thinking we might have a cold or something similar.
My wife, a special education teacher, went to work the next morning. She had planned an overnight camping trip with a group of students. Knowing they could not go without her, she soldiered on. I felt much worse and decided to take the day off. On top of that, I was supposed to take care of our children while my wife was away.
Still exhausted, I developed a fever, headache, chills, shortness of breath, and, soon, a cough. It had been 28 years since my last bout with pneumonia, and I didn’t put two and two together right away. This was pre-COVID, so I thought I had the flu or some other virus.
As my fever climbed to over 103, I was in a fog. I remember driving to pick up my daughter from school and running a red light. It was one of those things where you say, “What did I just do?” a split second after doing it. I could have killed myself or someone else. I was extra careful on the drive home.
At the house, I had trouble putting the key into the door. I’m not sure if I was delirious or what, but I decided this was something more serious than the flu.
I called the campground, and they tracked my wife down. I told her about running the light, the temperature I could not keep down, the cough, and the total lack of energy. I asked if she could come home so I could go to the emergency room. She couldn’t without having to pull her students from the camp. She recommended I call a friend of hers to watch the kids while I went to the hospital.

Pneumonia can be deadly
The ER doctor concentrated on bringing my fever down and hydrating me with an IV. She said my lungs seemed clear. She didn’t take an X-ray and just used the stethoscope. Despite my struggles to breathe, my pulse oximeter reading must have been acceptable. She seemed unalarmed, and I couldn’t help but feel she was not grasping the seriousness of the situation.
Several hours later, after the IV, she proclaimed me fit enough to go home, telling me to stay hydrated and to take Tylenol for the fever. I arrived home to the kids in bed. Thankful, I crawled into my bed and attempted to sleep through the coughing.
The next day, I was worse. I could barely move, and my fever climbed as high as 105 in between doses of Tylenol. By the time my wife came home in the afternoon from her camping trip — after stopping to pick up our children — she took one look at me and said, “You are going back to the hospital.”
So, the whole family packed up and took a road trip to the ER. This time, I was intent on conveying the seriousness of my symptoms. “I feel like I’m about to die,” I told the new ER doctor.
He ran some tests and conducted X-rays. A few hours later, he told me he suspected I had pneumonia and that I should not have been sent home the previous night. He admitted me that night, and it took 6 days of antibiotics, IVs, and breathing therapy for me to recover enough to return home.
My diagnosis led my wife to visit her doctor the next day, where she was diagnosed with the same condition. Her friends pitched in to help with the kids. And she, ever the trooper, managed her symptoms at home throughout my hospital stay.
Looking back on it, I don’t know if my most recent bout of pneumonia stands out as the worst because it really was the worst, or because it’s the one I remember best. I do know it is pretty serious to spend 6 days in the hospital in this day and age when they want you out the day after surgery or childbirth.
I avoided the vomiting of my childhood. But the complete lack of energy, muscle aches, chills, headache, fever, and cough were debilitating. It was the sickest I’ve ever been, and, as I told the ER doctor, I truly felt like I was dying.
Most healthy people with pneumonia get better in a few weeks if they receive the right treatment. However, for some people, pneumonia can be dangerous and even life-threatening. About 50,000 U.S. adults die from it every year.
After six battles with pneumonia, I want no part of a seventh.

Why trust our experts?