Key takeaways:
Community-acquired pneumonia (CAP) is a common lower respiratory tract infection of the lungs.
Symptoms of CAP include cough, fever, chills, and trouble breathing.
Antibiotics treat CAP caused by bacterial infection. Getting early treatment can keep you from developing a more serious lung infection.
Community-acquired pneumonia (CAP) is a lung infection caused by bacteria and viruses.
CAP is what most people think of when they hear the term “pneumonia.” The “community-acquired” part sets it apart from the types of pneumonia people get when they’re in a healthcare setting, like hospital-acquired pneumonia and ventilator-associated pneumonia.
Millions of people get CAP every year, making it one of the most common lower respiratory tract infections.
What causes community-acquired pneumonia?
Both bacteria and viruses cause CAP. Some important bacteria that cause CAP are:
Streptococcus pneumoniae: Even with pneumonia vaccines, this is still the most common cause of bacterial pneumonia. It’s where the word “pneumonia” comes from.
Mycoplasma pneumoniae: This bacteria is best known for causing walking pneumonia, especially in children and young adults.
Common viral causes of CAP include:
Influenza (the flu)
How do you get community-acquired pneumonia?
People develop CAP when viruses and bacteria pass from their nose and mouth into their lungs.
The bugs that cause CAP also cause upper respiratory tract infections, including the common cold. In many cases, people start off with more mild illnesses and then develop pneumonia as the bacteria or virus invades the lungs.
Scientists are still learning why some people develop pneumonia while others don’t, even if they’re sick with the same bacteria or virus.
Lower respiratory tract infections: Find out how pneumonia, bronchiolitis, and bronchitis differ — and how to manage each of them.
Who should get a pneumonia vaccine? Learn about pneumococcal vaccines and if you’re a candidate to receive one.
You don’t always need antibiotics to treat a cough. Here’s when you should take antibiotics for a cough and when you can treat your cough at home.
Babies, young children, and older adults are more likely to develop CAP. People who have chronic lung conditions or weakened immune systems are also at higher risk of developing CAP.
What are the symptoms of community-acquired pneumonia?
Symptoms of CAP vary from person to person. Some people have more severe symptoms and get sick all of a sudden. Others have more subtle symptoms that come on more gradually.
Most people notice:
Fever
Cough
Chest pain when taking in a breath
Shortness of breath
Rapid breathing
Trouble breathing
Chills
Fatigue
- ZithromaxAzithromycin
- ActiclateDoxycycline Hyclate
- MorgidoxDoxycycline Hyclate
The pattern of your symptoms can give you important clues. If you’ve been sick with a cold, signs you may have developed CAP include:
Symptoms that are getting worse instead of better over time
A fever that started in the middle of your illness
Trouble breathing or shortness of breath that developed all of a sudden or slowly over several days
People older than age 65 may have more subtle symptoms of pneumonia. For example, they may not develop a fever or cough and instead have symptoms like:
Confusion
Loss of appetite
Malaise
How do you diagnose community-acquired pneumonia?
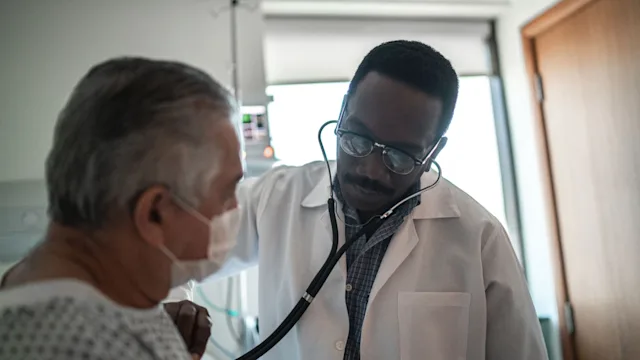
Your primary care provider may be able to tell if you have CAP just by listening to your lungs and asking you about your symptoms. A chest X-ray can also help diagnose pneumonia, but it’s not always necessary.
Some people need additional tests if they’re very ill and need care in the hospital.
How do you treat community-acquired pneumonia?
Antibiotics can treat CAP that a bacteria causes. But antibiotics won’t help if a virus is the cause of your pneumonia.
Even so, most healthcare professionals will prescribe a course of antibiotics just to be safe. That’s because it’s not always easy to tell if a bacteria or virus is the cause of CAP.
Common antibiotic treatments for CAP include:
Amoxicillin / clavulanate (Augmentin)
Azithromycin (Zithromax)
Levofloxacin (Levaquin)
People need to take antibiotics for at least 5 days. People with certain medical conditions may need to take antibiotics for longer.
People who are very sick and need care in the hospital often receive antibiotics through an IV line.
How do you prevent community-acquired pneumonia?
There are several things you can do to lower your risk of developing CAP.
The same healthy habits that can keep you from getting sick with common viruses can also help you avoid pneumonia:
Wash your hands often.
Avoid touching your face and nose.
Clean and disinfect frequently touched surfaces.
Avoid people who are sick with a cold, flu, or COVID.
Consider wearing a mask in public places if there’s a lot of virus activity in your community.
Two additional things you can do to keep your lungs safe from CAP include:
Quitting smoking: People who smoke are more likely to develop CAP. Secondhand smoke also increases the risk of developing pneumonia in kids. If you smoke, consider quitting. It’ll protect you as well as your loved ones.
Getting vaccinated: There are several pneumococcal vaccines that help prevent pneumonia including — pneumococcal polysaccharide vaccine (PPSV23) and pneumococcal polyconjugate vaccines (PCV15, PCV20, and PCV21). The pneumococcal vaccine is part of the routine childhood vaccination schedule. The CDC also recommends that all people over age 50 get a pneumococcal vaccine. People with weakened immune systems, cochlear implants, or asplenia may need additional doses of these vaccines at different times in their lives.
When to see seek care for pneumonia
You should see a healthcare professional if you think you might have pneumonia. CAP can often be diagnosed in an office visit, based on your symptoms and physical exam. Most people can complete treatment for CAP at home.
In some cases, though, you might need treatment in a hospital for CAP. Examples are if you have underlying lung, heart, or kidney issues, or if you have a severe infection.
Signs of severe CAP include:
Temperature less than 95°F or greater than 103.8°F
Respiratory rate greater than 30 breaths per minute (bpm)
Low blood pressure
Elevated heart rate
Abnormal labs like low sodium or elevated blood sugar
Frequently asked questions
Walking pneumonia is a term to describe mild CAP. People with mild CAP generally feel well enough that they’re still “walking around” despite having the infection. The virus or bacteria that cause walking pneumonia can spread from person to person.
Pneumonia can be life-threatening. Older patients and people with chronic medical conditions that weaken the lungs or immune system are at higher risk for severe CAP. The mortality rate among adults hospitalized with CAP is about 6%.
Yes, it’s possible to have pneumonia without developing a fever. People with mild cases of CAP may not have an elevated temperature. And older adults sometimes don’t get a fever with infection.
Walking pneumonia is a term to describe mild CAP. People with mild CAP generally feel well enough that they’re still “walking around” despite having the infection. The virus or bacteria that cause walking pneumonia can spread from person to person.
Pneumonia can be life-threatening. Older patients and people with chronic medical conditions that weaken the lungs or immune system are at higher risk for severe CAP. The mortality rate among adults hospitalized with CAP is about 6%.
Yes, it’s possible to have pneumonia without developing a fever. People with mild cases of CAP may not have an elevated temperature. And older adults sometimes don’t get a fever with infection.
The bottom line
CAP is a lung infection caused by viruses and bacteria. Symptoms include cough, fever, and trouble breathing. Some people have symptoms that start all of a sudden while others notice colds that get worse over time.
Antibiotics can cure pneumonia caused by a bacterial infection. To avoid getting sick, wash your hands often and avoid contact with people who are sick. There are vaccines that prevent pneumonia. Talk to your primary care provider about whether you’re a candidate for a pneumonia vaccine.

Why trust our experts?



References
American Cancer Society. (2019). Health risks of secondhand smoke.
American Lung Association. (2023). 3 things to know on World Pneumonia Day.
Baskaran, V., et al. (2019). Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PLoS One.
BMJ Best Practice. (n.d.). Community-acquired pneumonia in adults (non Covid-19).
Centers for Disease Control and Prevention. (2024). Pneumococcal vaccine recommendations.
Dickson, R. P., et al. (2014). Towards an ecology of the lung: New conceptual models of pulmonary microbiology and pneumonia pathogenesis. The Lancet.
File, T. M., Jr. (2012). Community-acquired pneumonia, bacterial. Netter’s Infectious Diseases. Elsevier.
Fung, H. B., et al. (2010). Community-acquired pneumonia in the elderly. The American Journal of Geriatric Pharmacotherapy.
MD Calc. (n.d.). PSI/PORT score: Pneumonia severity index for CAP.
Metlay, J. P., et al. (2019). Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine.
Ramirez, J. A., et al. (2017). Adults hospitalized with pneumonia in the United States: Incidence, epidemiology, and mortality. Clinical Infectious Diseases.
Regunath, H., et al. (2024). Community-acquired pneumonia. StatPearls.
Womack, J., et al. (2022). Community-acquired pneumonia in adults: Rapid evidence review. American Family Physician.