Key takeaways:
Aspiration pneumonia is a lung infection that happens when contents from the mouth or stomach enter the lungs.
The most common causes are swallowing issues, decreased alertness, and chronic medical problems.
Treatment for aspiration pneumonia includes antibiotics and supportive care. Prevention can also be very effective.
Pneumonia is a lung infection caused by bacteria, viruses, or fungi. Anyone can get pneumonia. But it’s most common in very young children and older adults. People with weak immune systems and chronic medical problems are also more at risk. Aspiration pneumonia is a bacterial lung infection with a specific cause — an aspiration event.
What is aspiration pneumonia?
During an aspiration event, stomach or mouth contents accidentally travel past the vocal cords and down into the trachea (windpipe). From there, it can easily enter the lungs, which people often describe as something “going down the wrong pipe.” These contents typically include things like:
Saliva
Food
Drinking liquids
Vomit
Once in the lungs, the aspirated contents can irritate the lung tissues. Bacteria are usually present when you aspirate because they live in the mouth and nose. The lungs are normally a sterile environment. So, if bacteria enter through aspiration, this can start an infection and lead to pneumonia.
What causes aspiration pneumonia?
Aspiration pneumonia usually happens when the body’s natural defenses fail to keep food, liquid, or stomach contents out of your airway. Normally, protective reflexes like coughing and the vocal-cord structures prevent materials from entering your lungs. When those defenses are impaired, aspirated material can reach your lungs and trigger an infection. This most often stems from problems with swallowing or a lowered level of alertness. Common situations include:
Swallowing problems (dysphagia): This is often due to conditions like stroke, which affect the nerves and muscles of the throat.
Decreased alertness: Sedation, anesthesia, alcohol or drug intoxication, or coma can weaken your protective reflexes.
Seizures: Seizure activity can cause sudden loss of airway protection and increase the risk of inhaling saliva, vomit, or food.
Vomiting or reflux: Stomach contents may move backward into the airway, especially with acid reflux or during pregnancy and labor.
Blockages or narrowing of the esophagus: Structural problems make it easier for material to go down the “wrong pipe.”
What are signs and symptoms of aspiration pneumonia?
In general, the most common symptoms of aspiration pneumonia are similar to any other type of pneumonia. They include:
Fever
Difficulty breathing
Wheezing
Cough
Chest pain
Low energy
Confusion, especially in older adults
The severity of an aspiration event can widely vary. Some aspirations go unnoticed and include small amounts of material multiple times per day. Others may include choking, gagging, or a coughing event followed by immediate symptoms.
Treatment for pneumonia will depend on what’s causing your infection. These common pneumonia treatments can help you feel better soon.
There are many reasons you might develop pneumonia. Find out the most common causes and how you can prevent it.
Could it be pneumonia? Take this quiz to see if your symptoms are more likely to be pneumonia versus bronchitis.
Immediate symptoms can include coughing that won’t go away or difficulty breathing. But these are usually a sign of lung irritation (pneumonitis) — not infection. In most cases, aspiration pneumonia doesn’t develop until 24 to 48 hours after an aspiration event. By then, the bacteria have had time to grow and cause pneumonia.
Who gets aspiration pneumonia?
Anyone can get aspiration pneumonia, but there are several risk factors.
People with swallowing issues
Many conditions can affect the ability to swallow normally. These often include diseases involving the nerves and muscles of the head and neck. Conditions that can cause weakness of the muscles of the mouth, throat, and esophagus are:
Cerebral palsy
- ZithromaxAzithromycin
- ActiclateDoxycycline Hyclate
- MorgidoxDoxycycline Hyclate
People with decreased consciousness
A reduced level of alertness can interfere with your protective reflexes against aspiration. Possible causes of decreased alertness include:
Coma
General anesthesia or deep sedation
Alcohol or drug intoxication
Seizures
People with coexisting medical conditions
Medical conditions that increase the risk of vomiting can make an aspiration more likely. Some examples include:
Narrowing of the esophagus
Obesity
Pregnancy and labor
How do you diagnose aspiration pneumonia?
Diagnosing aspiration pneumonia begins with identifying the pneumonia. And then a healthcare professional will often look for the cause. When looking for possible causes of pneumonia, your healthcare team will always consider aspiration. This is especially true in those who are older or have other risk factors.
There are different tools to diagnose pneumonia, including:
Medical history: Your symptoms, medical conditions, and a history of similar problems are useful. They help give your healthcare team context to the situation.
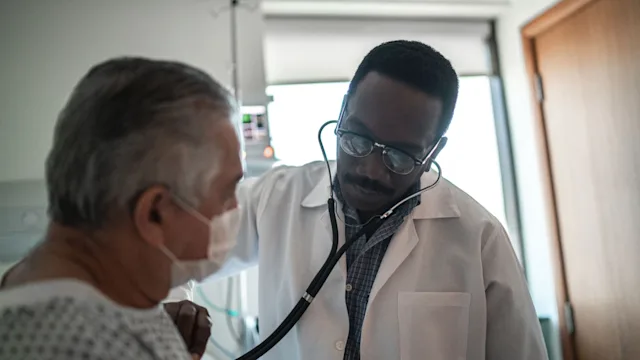
Physical exam: Listening to your chest with a stethoscope may identify abnormal lung sounds. Your vital signs and oxygen levels can alert a healthcare professional of breathing issues.
Lab studies: Special blood tests and bacterial cultures help look for signs of infection.
Chest X-ray: A chest X-ray can show areas of the lungs filled with infection.
Chest CT: In some cases, a chest CT may be needed to look more closely at the lungs.
Bronchoscopy: Bronchoscopy is a medical procedure used to look for evidence of aspirated material or infection through a sample of lung fluids.
What are the treatments for aspiration pneumonia?
Aspiration pneumonia is caused by bacteria. And one of the most important treatments is antibiotics. The type of antibiotic that’s best will depend on the bacteria most likely causing the infection.
In addition to antibiotics, supportive care is often necessary until the pneumonia improves. This can include:
Fever control
Hydration
Rest
Oxygen
Breathing treatments
Intubation (breathing tube)
Even with treatment, aspiration pneumonia can be dangerous. In fact, the risk of death can be up to 30%. Recognizing the signs and starting treatment early may help improve recovery.
Preventing aspiration pneumonia is also key — especially for those most at risk.
How to prevent aspiration
Not every aspiration event can be avoided, but there are steps that can lower the risk, especially for people who are at higher risk of aspiration pneumonia. Here are some helpful strategies:
Address swallowing problems. A speech or swallowing therapist can teach techniques to make swallowing safer.
Sit upright when eating or drinking. Staying upright during meals and for 30 to 60 minutes afterward helps food and liquid move down properly.
Eat slowly and take small bites or sips. This gives the muscles and reflexes more time to coordinate swallowing.
Adjust medications if needed. Some sedatives or muscle relaxants can make aspiration more likely. Talk with your healthcare team if this is a concern.
Use feeding tubes when necessary. In severe swallowing disorders, a feeding tube may be recommended to reduce the risk of aspiration.
Prevention strategies are most effective when tailored to the individual’s needs, so working with your healthcare team is key.
Frequently asked questions
The chances of survival depend on your overall health, age, and the severity of your infection. Aspiration pneumonia can be serious — with mortality rates around 10% to 20% for people who are in the hospital. But most people who are otherwise healthy tend to recover well with timely treatment. Getting medical care early, taking prescribed antibiotics as directed, and following your healthcare team’s guidance can make a big difference in recovery.
Most people start feeling better within 1 to 3 weeks, though full healing can take longer depending on your age and overall health. Chest X-rays often show improvement more slowly than symptoms, which can take up to a month to fully clear. Recovery may take longer if there are complications or if you have other lung or medical conditions.
No. Aspiration pneumonia is caused by food, liquid, saliva, or vomit entering the lungs, not by catching it from another person. The infection develops from bacteria that are already in the mouth or stomach. Because of this, aspiration pneumonia doesn’t spread from person to person the way flu or viral pneumonia can. Good oral hygiene and medical management of swallowing problems are the best ways to reduce your risk.
The chances of survival depend on your overall health, age, and the severity of your infection. Aspiration pneumonia can be serious — with mortality rates around 10% to 20% for people who are in the hospital. But most people who are otherwise healthy tend to recover well with timely treatment. Getting medical care early, taking prescribed antibiotics as directed, and following your healthcare team’s guidance can make a big difference in recovery.
Most people start feeling better within 1 to 3 weeks, though full healing can take longer depending on your age and overall health. Chest X-rays often show improvement more slowly than symptoms, which can take up to a month to fully clear. Recovery may take longer if there are complications or if you have other lung or medical conditions.
No. Aspiration pneumonia is caused by food, liquid, saliva, or vomit entering the lungs, not by catching it from another person. The infection develops from bacteria that are already in the mouth or stomach. Because of this, aspiration pneumonia doesn’t spread from person to person the way flu or viral pneumonia can. Good oral hygiene and medical management of swallowing problems are the best ways to reduce your risk.
The bottom line
Everyone has felt something “go down the wrong pipe” when swallowing. In most cases, the body’s reflexes can clear the issue and nothing harmful happens. But people who have trouble swallowing or decreased alertness can get aspiration pneumonia. And this can be dangerous if untreated. If you have signs and symptoms of aspiration, let a healthcare professional know right away.

Why trust our experts?



References
American Lung Association. (2025). Pneumonia symptoms and diagnosis.
Kosutova, P., et al. (2021). Aspiration syndromes and association lung injury: Incidence, pathophysiology and management. Physiological Research.
Lanspa, M. J., et al. (2012). Mortality, morbidity, and disease severity of patients with aspiration pneumonia. Journal of Hospital Medicine.
Sanivarapu, R. R., et al. (2024). Aspiration pneumonia. StatPearls.
Son, Y. G., et al. (2017). Pneumonitis and pneumonia after aspiration. Journal of Dental Anesthesia and Pain Medicine.