Key takeaways:
Many types of strokes can happen, including ischemic strokes, hemorrhagic strokes, and transient ischemic attacks (ministrokes). Each is treated in different ways.
Depending on the type of stroke you have, you may be prescribed multiple medications to help lower your risk of having another stroke.
How long you need to take medication to help lower your risk of having another stroke will depend on many factors.
Save on related medications
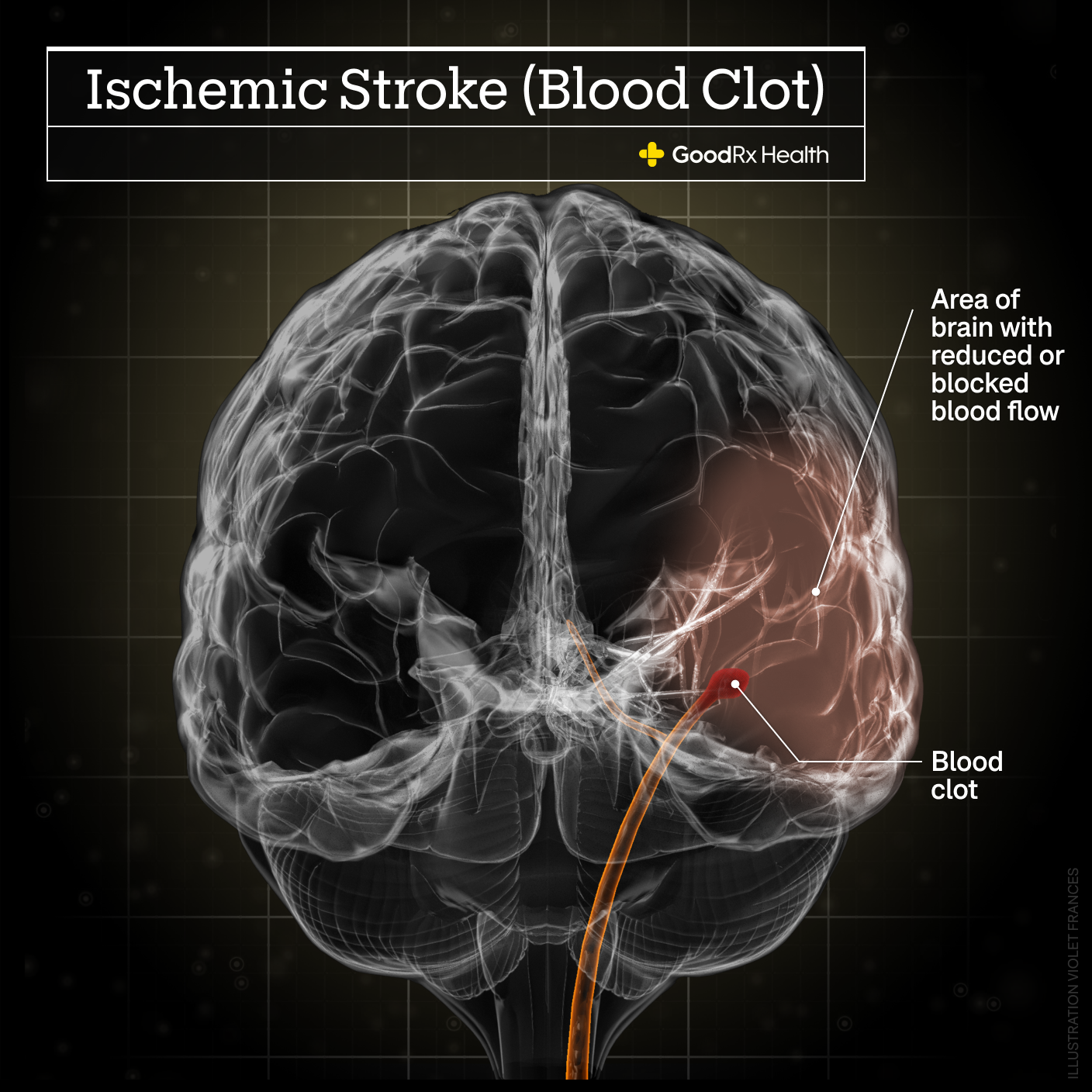
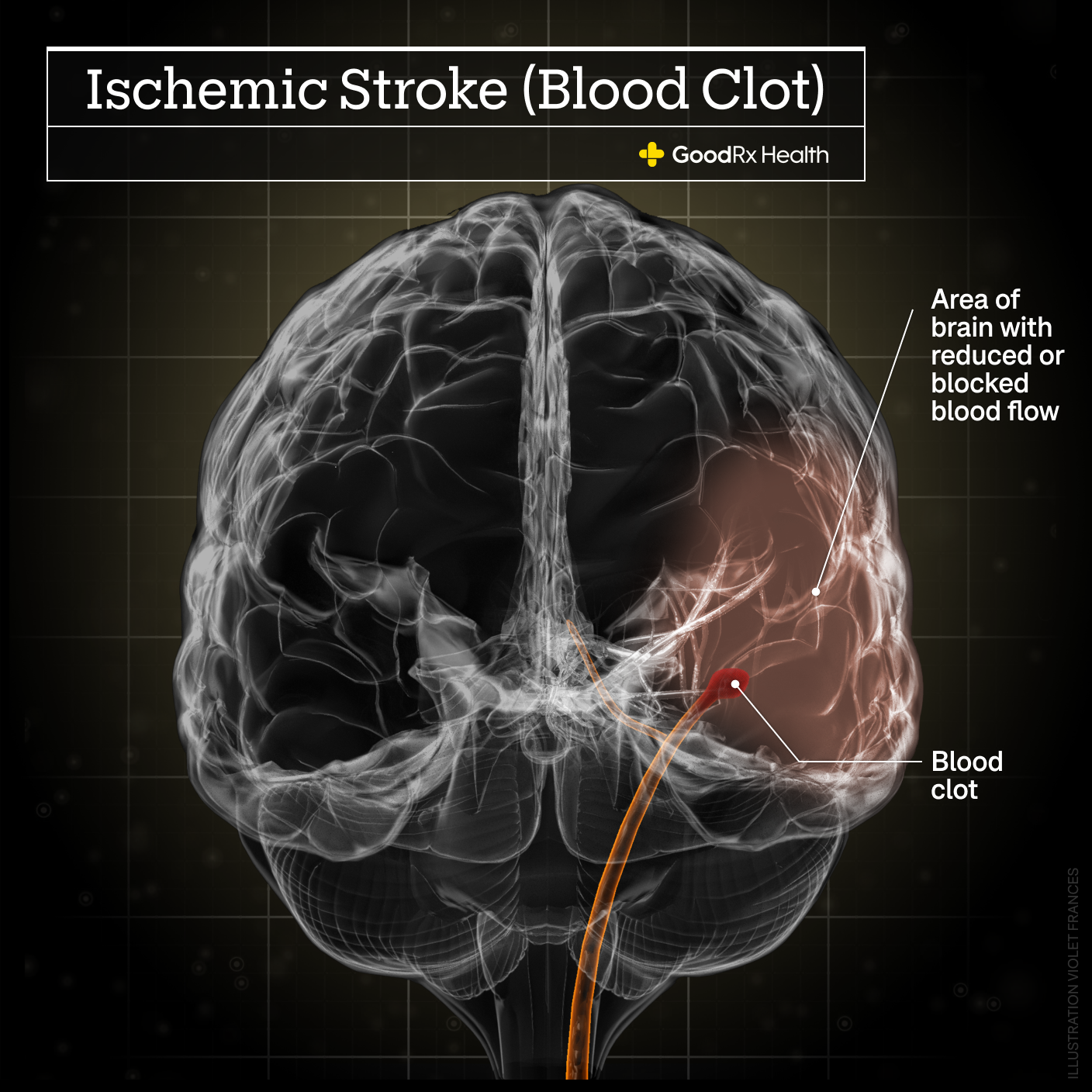
A stroke is when blood doesn't flow correctly in your brain. This prevents oxygen and nutrients from reaching your brain cells. Those brain cells then die.
Strokes can be dangerous and cause permanent brain damage. Once this happens, you may need physical therapy to do what you used to, like walking, speaking, or even eating.
But even after having a stroke and recovering, you may be at risk for a future stroke. In fact, 1 in 4 stroke survivors may have another one within 5 years. Because of this risk, there’s a big focus on preventing strokes from happening again. More likely than not, you'll be prescribed medications to help prevent a future stroke.
Here, we’ll discuss the medications commonly prescribed after a person has had a stroke.
What medications are typically prescribed after a stroke?
There are several medications your healthcare provider may prescribe after you have a stroke. These medications can help lower your risk of having one again. Which ones you’re prescribed will depend on several factors.
First, your healthcare provider must determine what type of stroke you had. There are three main types of strokes:
Ischemic stroke: This is where a blood clot gets stuck in a blood vessel in your brain. These clots could come from fat deposits in your blood vessels. They can also come from your heart due to an abnormal heart rhythm, such as atrial fibrillation.
Hemorrhagic stroke: This is where a blood vessel in your brain ruptures and blood builds up in your brain.

Transient ischemic attack (TIA): This is sometimes called a ministroke. This is where blood flow in the brain is blocked for a small amount of time and causes stroke-like symptoms (e.g., dizziness, trouble balancing, numbness on one side of the body).
After your healthcare provider knows what type of stroke you’ve had, they’ll look at other health conditions you may have. Certain medical conditions raise your risk of having a stroke again. Examples include high blood pressure, high cholesterol, and diabetes.
Your provider will need to make sure these conditions are being treated appropriately. You may be asked to follow up with your provider later to have these conditions more closely evaluated. However, treating these other conditions can add to the number of medications you’re prescribed.
Everyone’s post-stroke medication regimen may be different. But there are some standard stroke medications you may be prescribed.
Read more like this
Explore these related articles, suggested for readers like you.
Antiplatelets
Platelets are important blood cells that form clots to help stop bleeding. Usually, clotting is a good thing; like when you have a cut on your finger, platelets help stop the bleeding. But, if clots form and get stuck in your brain blood vessels, then a stroke can happen.
Antiplatelet medications help prevent platelets from sticking together and making clots. There are several antiplatelet medications available. Depending on the details of your stroke, you could be prescribed one or more antiplatelet.
Commonly prescribed antiplatelets include:
Aspirin/dipyridamole (Aggrenox)
Clopidogrel (Plavix)
Ticagrelor (Brilinta)
Anticoagulants
Anticoagulants are commonly called blood thinners. These medications can also help prevent clots from forming — but in a different way. Antiplatelets stop platelets from sticking together. Anticoagulants stop red blood cells from sticking together.
When you have an abnormal heart rhythm, such as atrial fibrillation, blood can get stuck in the heart. After some time, those blood cells can start to stick together and form a blood clot. If this clot gets pumped out of the heart, it can travel and get stuck in brain blood vessels. This can cause a stroke.
Anticoagulants can help prevent these types of clots from forming. If your stroke was caused by atrial fibrillation, you’ll likely be prescribed an anticoagulant medication.
Some commonly prescribed anticoagulant medications include:
Warfarin (Coumadin, Jantoven)
Dabigatran (Pradaxa)
Apixaban (Eliquis)
Rivaroxaban (Xarelto)
In rare cases, your provider may have you take both an antiplatelet and an anticoagulant. This depends on several factors, including the type of stroke you had.
Are there other medications you may need?
Possibly. As discussed earlier, you may need other medications depending on other conditions you have. If you have a medical condition that raises the risk of having another stroke, you may also be prescribed medications to help treat it. The following are commonly used medications, but this doesn’t cover all possibilities you could face.
High blood pressure medications
High blood pressure (hypertension) can raise your risk of having a stroke. If your blood pressure is high, you could be prescribed one or more blood pressure medications after a stroke. If you’re already taking blood pressure medications, your healthcare provider may change your doses or switch medications.
Blood pressure medications that may be prescribed after a stroke include:
Thiazide diuretics (water pills), such as hydrochlorothiazide (Microzide)
Angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril (Prinivil, Zestril)
Angiotensin II receptor blockers (ARBs), such as losartan (Cozaar) and valsartan (Diovan)
The American Heart Association (AHA) recommends using medications to keep blood pressure below 130/80 mmHg. Several studies suggest that keeping your blood pressure under this number helps lower your risk of a future stroke.
High cholesterol medications
Another condition you’ll be checked for after a stroke is high cholesterol. When cholesterol is too high, it raises your risk of a stroke. Healthcare providers keep a particularly close eye on one type of cholesterol: low-density lipoprotein (LDL, or bad cholesterol).
If your LDL is over 100 mg/dL, the AHA recommends taking atorvastatin (Lipitor) 80 mg once a day. If you also have other heart problems, such as heart disease, you may be prescribed atorvastatin along with another cholesterol medication called ezetimibe (Zetia). Your healthcare provider may also recommend that you try to keep your LDL under 70 mg/dL.
Diabetes medications
Diabetes can raise your risk of a stroke. Controlling your blood sugar helps lower this risk. If you have uncontrolled diabetes, your healthcare provider may change your current diabetes medication regimen after having a stroke. There are many different types of diabetes medications and treatments available. Speak with your healthcare provider to discuss the best way for you to treat this condition.
How long do you have to take medication after having a stroke?
This depends on many factors. The most important thing to know about strokes is that there are many types of them. Strokes can have several different causes and happen in different parts of your brain. Your provider will do a lot of tests before setting up a treatment plan for you. This plan will likely include lifestyle changes and medication for a period of time.
You may need to take some medications only for a few months. Other medications may need to be taken for years after a stroke. It’s also possible that some people will stay on certain medications long term. Make sure to go for any tests your healthcare provider recommends. These tests will help them decide how long you should continue taking your medications.
If you’ve been prescribed medications for other health conditions, like diabetes, you may take them long term. These other conditions are typically chronic and often require life-long treatment.
What happens if you stop taking post-stroke medications?
If you stop taking your post-stroke medications without your healthcare provider’s OK, it can raise your risk of having another stroke. Don’t stop taking your medications unless your healthcare provider tells you to do so. If you’re experiencing bothersome side effects, let your healthcare provider know. They may suggest ways to lessen these side effects without completely stopping your medications.
The bottom line
Strokes can be very scary, and many people wonder what they need to do after having one. Medications play a large role in helping to lower your risk of having another stroke. What medications your provider will prescribe for you will depend on the type of stroke you had and other health conditions you may have. It’s important to take your medications as prescribed to help lower the risk of another stroke.

Why trust our experts?



References
American Diabetes Association. (2021). Stroke.
American Heart Association. (2016). Atrial fibrillation medications.
American Heart Association. (2016). Health threats from high blood pressure.
American Heart Association. (2016). Why atrial fibrillation (AF or AFib) matters.
American Heart Association. (2018). My life check | Life's simple 7.
American Heart Association. (2020). HDL (good), LDL (bad) cholesterol and triglycerides.
American Heart Association. (2021). About stroke.
American Heart Association. (2021). Risk factors under your control.
American Heart Association. (2021). Types of stroke and treatment.
Centers for Disease Control and Prevention. (2021). Stroke.
Centers for Disease Control and Prevention. (2021). Stroke facts.
Centers for Disease Control and Prevention. (2021). Stroke treatment.
Kleindorfer, D. O., et al. (2021). 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke.
National Library of Medicine. (2021). Transient ischemic attack.
OneBlood. (2019). What are platelets?.
U.S. National Library of Medicine. (2021). Stroke.