Key takeaways:
Medicare Part B pays for medically necessary cataract surgery, as does Medicare Advantage.
Cataract surgery could cost someone on Medicare as little as $320 out of pocket.
It usually costs less to have the procedure done at an ambulatory surgery center than a hospital.
Cataracts affect an estimated 60% of people age 65 or older in the U.S., and surgery is the main remedy. So it’s no surprise that Medicare covered more than 14 million cataract surgeries between 2011 and 2019. One study estimated that more than 80% of people getting cataract surgery are on Medicare.
What is cataract surgery?
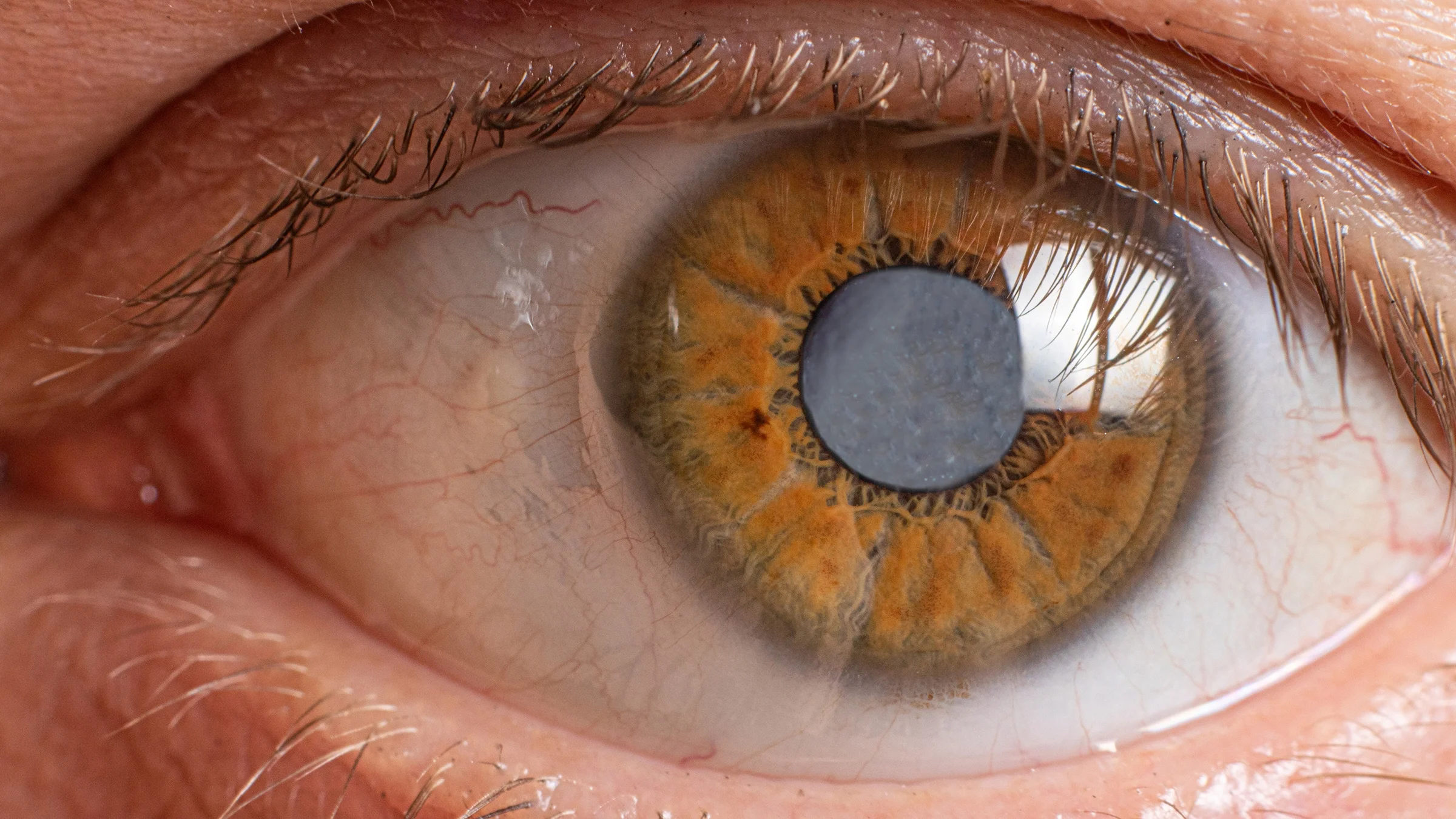
Cataracts occur when proteins in the lenses of your eyes break down, causing your vision to get cloudy. Cataract surgery replaces your eye’s foggy natural lens with a clear artificial lens, called an intraocular lens or IOL.
The surgery usually takes place on an outpatient basis. It’s low risk and relatively quick (about 10 minutes per eye).
Search and compare options
If both eyes have cataracts, the procedure is usually done one eye at a time, with operations at least a month apart. This schedule makes for easier recovery and reduces the chance of complications.
What are the costs of cataract surgery?
For people with original Medicare, the national average price of cataract surgery at an ambulatory surgical center (ASC) is $1,606. The out-of-pocket cost can be as little as $320.
That said, several factors can affect your personal medical bill. These include:
Choice of facility: Surgery at an ambulatory surgical center typically costs hundreds of dollars less than at a hospital outpatient facility.
Type of surgery: There are two commonly used techniques for cataract surgery. Phacoemulsification (“phaco”) uses a small incision; extracapsular cataract extraction (ECCE) uses a larger one. A Medicare beneficiary’s average ASC price is $361 for ECCE or $369 for phaco.
Type of artificial lens: Medicare only covers one type of IOL: the standard monofocal lens, which provides clear vision at one distance. But there are different types of IOLs. If you choose an advanced multifocal lens (to see near and far), it could cost you thousands of dollars out of pocket.
Potential post-surgery expenses: These can sometimes be costly. For instance, retinal detachment is a common complication. For surgery to repair it, a Medicare patient’s out-of-pocket cost can range from hundreds of dollars to more than $1,000. The total cost depends on the type of procedure.
What does Medicare cover for cataract surgery?
Medicare covers these elements of cataract surgery:
The removal of the cataract: This may be done with traditional techniques or lasers.
Basic lens implants: Medicare covers only conventional monofocal lenses that improve eyesight at one distance.
One set of eyeglasses or contact lenses after the surgery: Medicare covers standard frames only. If you decide to get premium frames instead, Medicare won’t pay for the upgrade.
Does Medicare pay for anesthesia and sedation?
Anesthesia is covered by Medicare Part B or Medicare Advantage (Part C).
Read more like this
Explore these related articles, suggested for readers like you.
Under Part B, the medical insurance portion of Medicare, you’re charged 20% coinsurance for anesthesia. With Part C, the coinsurance share varies by plan. Moderate sedation, where the person is awake, is considered a type of anesthesia and is likely to be covered as well.
What aspects of cataract surgery does Medicare not cover?
Medicare will pay costs associated with the placement and maintenance of a standard lens. But there are lenses that correct your vision for astigmatism or age-related presbyopia, and you may want one (or two) of those instead.
If you get a specialty lens, you may need additional treatments, services, or supplies for placing, adjusting, or monitoring it. But any cost that exceeds Medicare’s approved amount for standard cataract surgery and care won’t be covered. Instead, those extra costs will be billed to you.
Also, if you get a specialty IOL, Medicare will not pay for eyeglasses or contact lenses. Its reasoning is that a vision-correcting IOL does the jobs of both a standard IOL and a pair of prescription eyeglasses.
Can I find out how much Medicare will cover before I choose to have surgery?
Yes. The Centers for Medicare & Medicaid Services (CMS) offer a searchable database on outpatient procedure costs. That data tool can tell you the national average cost of cataract surgery and the amounts Medicare will pay. Keep in mind, though, that these prices are for people who:
Have original Medicare
Have already met their Part B deductible ($233 in 2022)
Do not have Medigap policies
After you reach your deductible, Part B pays 80% of the Medicare-approved amount. Your coinsurance share is 20%.
To be covered, your cataract condition must meet Medicare’s rules of medical necessity. CMS considers these factors in making its decision:
How severe is your condition? For example, a foggy lens without other symptoms may not qualify.
Do you also have other eye diseases?
How much is the cataract limiting your activity?
Does your documented medical history (including tests) confirm the necessity?
Which Medicare plans offer cataract surgery coverage?
Original Medicare’s Part B covers medical services specifically related to diagnosis and treatment of cataracts.
Medicare Advantage plans mirror the coverage under Medicare Parts A and B, but payments are provided by private insurers instead of the government. They are required to follow the same rules set by original Medicare.
So, if you have a Medicare Advantage plan and meet Medicare’s guidelines for medically necessary cataract surgery, you’ll be covered. Still, it’s wise to check your policy documents and contact your plan’s customer service reps to be sure.
Does my supplemental insurance cover the remaining costs of cataract surgery?
If you have original Medicare, you may also have Medicare supplement insurance (Medigap). Medigap helps pay for coinsurance, copays, and other out-of-pocket expenses.
For cataract surgery, any surgery charges or doctor fees beyond Medicare’s approved amounts can be paid through Medigap.
If you’re on a Medicare Advantage plan, though, you’re not allowed to have a Medigap policy. You are likely to end up paying coinsurance, copayments, and any excluded costs out of pocket.
How much will cataract surgery cost without supplemental coverage?
It depends on the type of Medicare coverage you have. Costs with Part B may differ from costs under Medicare Advantage due to additional rules in the Advantage plan.
With either type of plan, there’s one big way to keep costs down: Have your cataract surgery in an ASC rather than a hospital outpatient setting. ASC facility fees are about half the price of hospital facility fees — so Medicare pays less, and your coinsurance amount goes down, too.
Citing national averages, CMS reports that traditional cataract surgery at an ASC includes physicians’ fees of $544 and facility fees of $1,062. After Medicare pays $1,284 (its 80% share), your bill is $320.
Doctor fees stay the same at a hospital, but the facility fee jumps to $2,120, with Medicare paying $2,131 (80%). The cost of your 20% coinsurance rises to $532.
What post-surgery benefits does Medicare provide to the cataract patient?
As part of the “surgical package” payment, Medicare covers follow-up doctor visits for 10 days post-procedure.
Medicare Part B will typically cover one pair of eyeglasses or contact lenses for people with standard IOLs.
Part D, which provides prescription drug coverage, covers post-surgical medicated eye drops. It may also cover topical antibiotics and steroids as needed. Check your plan’s formulary list to be sure.
If complications arise from cataract surgery, will Medicare cover the cost of treating those?
If Medicare finds it medically necessary to treat those complications, it will cover the costs.
Here’s an example: “Secondary cataracts” may cause your vision to get cloudy again, weeks or months after your cataract surgery. To fix it, doctors perform a posterior capsulotomy. Medicare covers this procedure, at an average beneficiary cost of about $115.
The bottom line
When Medicare confirms that your cataract surgery is medically necessary, it will cover the procedure. You will have to meet your deductible first, of course. After that, your out-of-pocket costs will vary depending on whether you’re enrolled in traditional Medicare, have supplemental Medigap insurance, or get coverage through a Medicare Advantage plan. Other factors that can affect the total cost are the surgical setting, surgical technique, and type of intraocular lens.

Why trust our experts?


References
Ambulatory Surgery Center Association, et al. (n.d.). Medicare cost savings tied to ambulatory surgery centers.
Boyd, K. (2022). What is a posterior capsulotomy? American Academy of Ophthalmology.
Centers for Medicare & Medicaid Services. (2005). CMS rulings.
Centers for Medicare & Medicaid Services. (2007). CMS rulings.
Centers for Medicare & Medicaid Services. (2021). 2022 Medicare Parts A and B premiums and deductibles/2022 Medicare Part D income-related monthly adjustment amounts.
Centers for Medicare & Medicaid Services. (2021). Medicare vision services. Medicare Learning Network.
Centers for Medicare & Medicaid Services. (2022). Chapter II: Anesthesia services.
Gurnani, B., et al. (2022). Phacoemulsification. StatPearls.
Humana. (2019). Medicare Parts A, B, C and D: Costs and coverage explained.
Malwankar, J., et al. (2021). Trends, factors, and outcomes associated with immediate sequential bilateral cataract surgery among medicare beneficiaries. Ophthalmology.
Maxwell, W. A., et al. (2008). A United States cost-benefit comparison of an apodized, diffractive, presbyopia-correcting, multifocal intraocular lens and a conventional monofocal lens. Journal of Cataract and Refractive Surgery.
Medicare.gov. (n.d.). Anesthesia.
Medicare.gov. (n.d.). Costs for Medicare Advantage plans.
Medicare.gov. (n.d.). Eyeglasses and contact lenses.
Medicare.gov. (n.d.). Find a Medigap policy that works for you.
Medicare.gov. (n.d.). Glossary.
Medicare.gov. (n.d.). Medicare Advantage plans cover all Medicare services.
Medicare.gov. (n.d.). Procedure price lookup.
National Eye Institute. (2022). Cataracts.
National Eye Institute. (2022). Retinal detachment.
U.S. Centers for Medicare & Medicaid Services. (2018). Global surgery booklet. Medicare Learning Network.
U.S. Centers for Medicare & Medicaid Services. (2019). Cataract extraction.
U.S. Centers for Medicare & Medicaid Services. (2022). Items and services not covered under medicare. Medicare Learning Network.
U.S. Centers for Medicare & Medicaid Services. (2022). Understanding Medicare Advantage plans.
University of Central Florida Health. (n.d.). What are secondary cataracts?
Zafar, S., et al. (2020). Prescribing patterns and costs associated with postoperative eye drop use in Medicare beneficiaries undergoing cataract surgery. Ophthalmology.
Zafar, S., et al. (2022). Endophthalmitis rates among Medicare beneficiaries undergoing cataract surgery between 2011 and 2019. Ophthalmology.