Key takeaways:
Psoriatic arthritis is a lifelong autoimmune condition that can cause inflammation in the skin (psoriasis), joints, spine, and tendons.
About 1 in 4 people who have psoriasis can one day develop psoriatic arthritis.
With treatment, the outlook for people with psoriatic arthritis is good. Many people live long, productive, and enjoyable lives with this condition.
Most people think of psoriasis as a condition that only affects the skin. While that’s true, about 1 in 4 people who have psoriasis can develop another condition called psoriatic arthritis (PsA). This is an autoimmune, inflammatory condition that affects the joints, tendons, and sometimes the eyes. So it’s important to keep an eye out for symptoms if you have psoriasis.
Psoriatic arthritis is different for everybody. In general, PsA is psoriasis rash plus joint pain and swelling. But, other symptoms can occur, too.
1. Joint pain or swelling
Psoriatic arthritis causes pain, swelling, and stiffness in the joints. It tends to be worse in the morning. PsA commonly affects the hands, but it can affect any joint in the body.
Here are some photos of joint swelling from psoriatic arthritis.

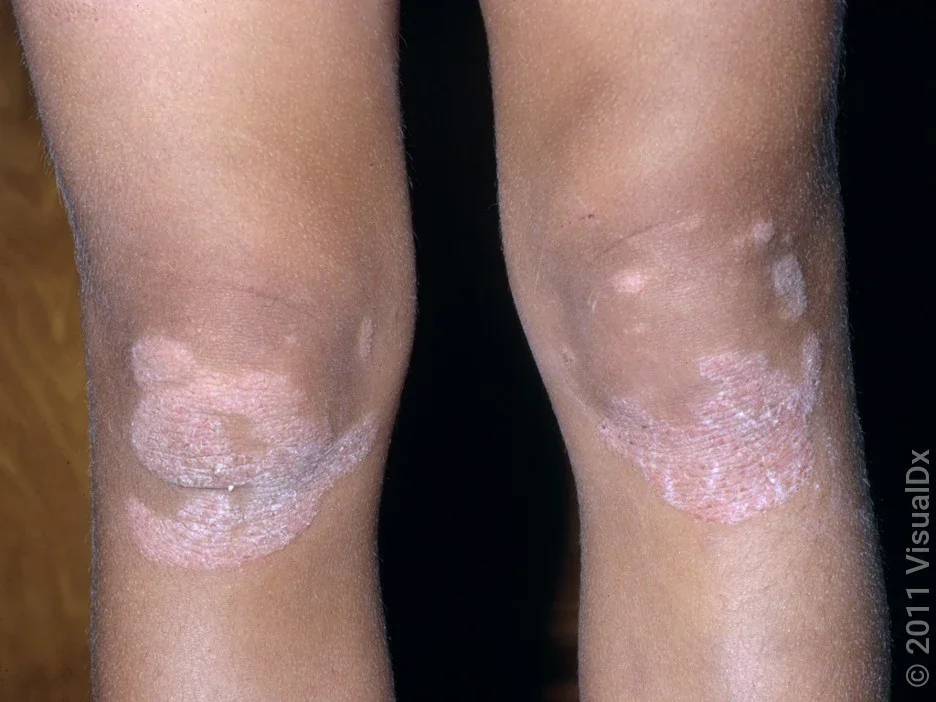
2. Skin rashes (psoriasis)
There are a few different types of psoriasis rashes. Red, scaly patches on the scalp, elbows, and knees are the most common. This is called plaque psoriasis. Psoriasis rashes can happen anywhere, including on the scalp, genitals, and buttocks.
Here’s a picture of plaque psoriasis in different skin tones.

3. Changes in the nails
Nail psoriasis can cause many different changes. They include color changes, ridges, tiny pits, or nails that appear crumbly. You may also see changes in the skin underneath the nails.
Here are some photos showing the different nail changes in psoriatic arthritis.


4. Pain and inflammation where tendons connect to bones
Entheses are areas where tendons connect to bone. Psoriatic arthritis can cause inflammation and pain in these areas, which is called enthesitis. The most commonly affected are at the back of the heel, elbows, and spine.
5. Pain and inflammation in the cartilage between the rib cage
This inflammation is called costochondritis. It causes chest pain that feels achy or pressure-like, and the area is usually very tender to touch. This pain might get worse when your rib cage expands to take a deep breath in or with movement of your arms.
Over time, psoriatic arthritis can damage the joints, skin, and eyes. The good news is, early treatment can help prevent these complications.
What’s it like to live with psoriatic arthritis? One person shares her experience with this diagnosis, and ways she practices self-care.
You can’t prevent or treat psoriatic arthritis with your diet alone. But you may notice a difference in your symptoms with a few diet changes.
6. Swelling of an entire finger or toe
This is also called “sausage digit” or dactylitis. In addition to swelling, it can also cause redness and warmth. It’s different from joint swelling because it affects the entire finger or toe.
Here’s a photo that shows two digits almost completely swollen from psoriatic arthritis.

7. Low back pain and stiffness
Psoriatic arthritis commonly causes back pain and stiffness throughout the spine. In particular, inflammation in the sacroiliac joints (where the pelvis meets the spine in the low back) is very common. This is called sacroiliitis.
- PrednisoneGeneric Deltasone and Rayos and Sterapred
- Exclusive discountAdalimumab-adbm
- OtezlaApremilast
8. Mid-back or neck pain and stiffness
This is due to inflammation in the spine itself (spondylitis). It commonly occurs with the low back pain of sacroiliitis, but it can occur alone about 25% of the time.
9. Eye inflammation
Psoriatic arthritis and psoriasis can cause a few different types of eye problems. These include blepharitis (inflammation of the eyelid) and conjunctivitis (inflammation of the eyelid lining).
Uveitis is a less common symptom of psoriatic arthritis. It’s due to inflammation of the uvea, which leads to:
Eye pain
Redness of the eye
Sensitivity to light
Blurry vision
10. Fatigue
Untreated inflammation in the body can make you feel run down, even when you get a decent night’s rest. So fatigue is a common symptom of most autoimmune conditions, including psoriatic arthritis.
What are the symptoms of a psoriatic arthritis flare?
A psoriatic arthritis flare is when symptoms temporarily get worse. Worsening rashes and joint pain are common during flares, but any of your symptoms can get worse. Sometimes new symptoms can also show up.
PsA flares can be triggered by infection, stress, and smoking. But they are different for everyone, since everyone has their own specific symptoms of PsA and their own triggers.
What are the early warning signs of psoriatic arthritis?
The early signs of psoriatic arthritis are the same as the symptoms listed above. Studies show that the earlier you get a PsA diagnosis and treatment, the better you’ll do in the long run. So it’s important to be aware of the early warning signs.
If you have psoriasis and develop any of these other symptoms, talk with your dermatologist or primary care provider. They can refer you to a rheumatologist (autoimmune specialist) who can determine if your symptoms are due to PsA or something else.
Is there anything I can do to prevent psoriatic arthritis?
If you have psoriasis, you’re probably wondering if there’s anything you can do to decrease your chances of getting psoriatic arthritis. Researchers aren’t sure why some people with psoriasis go on to develop PsA whereas others don’t. As of now, there are no medications that can prevent the development of psoriatic arthritis. But there are a few ways to keep your joints healthy as you age:
Stop smoking, if you smoke: Some research suggests that quitting smoking can improve psoriasis and decrease the chance of getting PsA in general, but the evidence is mixed. There are other health benefits of smoking cessation, too.
Maintain a balanced weight: A large study showed a link between carrying excess weight and an increased risk of developing PsA if you have psoriasis. So it can help to do your best to maintain a balanced weight through a nutritious diet and exercise.
Keep moving: Speaking of exercise, experts recommend regular exercise for all people and especially those with arthritis.
Be aware of joint pain and other symptoms: It’s important to pay attention to your body and let your healthcare team know if you experience new symptoms. Having psoriasis means you’re at greater risk for psoriatic arthritis, and the earlier it’s diagnosed and treated, the better.
Frequently asked questions
There isn’t one single test that diagnoses psoriatic arthritis. It’s usually a clinical diagnosis, which means a clinician can make the diagnosis based on your symptoms and physical examination. Sometimes imaging and blood tests are helpful.
The prognosis is pretty good — if you take your medications. There’s no cure for psoriatic arthritis, but living a healthy and fulfilling life is possible thanks to the many medications available to treat it. Treatments might include pills, infusions (into the vein), or injections (biologics).
If you don’t treat psoriatic arthritis, uncontrolled inflammation can lead to complications in the skin, joints, and other parts of the body. Taking your medication is the best way to protect your body from permanent complications of PsA.
Sometimes PsA is described in categories, based on which symptoms you have more of. They include:
Distal interphalangeal dominant, which mostly affects the knuckles closest to the fingernails
Asymmetric oligoarticular, which affects only a few joints with an unequal distribution between sides of the body
Symmetric polyarthritis, which affects several joints on both sides of the body
Spondylitis, which mainly affects the spine
Arthritis mutilans, which is more severe and causes joint damage and deformity
There isn’t one single test that diagnoses psoriatic arthritis. It’s usually a clinical diagnosis, which means a clinician can make the diagnosis based on your symptoms and physical examination. Sometimes imaging and blood tests are helpful.
The prognosis is pretty good — if you take your medications. There’s no cure for psoriatic arthritis, but living a healthy and fulfilling life is possible thanks to the many medications available to treat it. Treatments might include pills, infusions (into the vein), or injections (biologics).
If you don’t treat psoriatic arthritis, uncontrolled inflammation can lead to complications in the skin, joints, and other parts of the body. Taking your medication is the best way to protect your body from permanent complications of PsA.
Sometimes PsA is described in categories, based on which symptoms you have more of. They include:
Distal interphalangeal dominant, which mostly affects the knuckles closest to the fingernails
Asymmetric oligoarticular, which affects only a few joints with an unequal distribution between sides of the body
Symmetric polyarthritis, which affects several joints on both sides of the body
Spondylitis, which mainly affects the spine
Arthritis mutilans, which is more severe and causes joint damage and deformity
The bottom line
Psoriatic arthritis (PsA) is a lifelong but treatable autoimmune condition that typically affects the skin and joints. About 1 in 4 people with psoriasis will develop PsA. If you have psoriasis, it’s important to familiarize yourself with the symptoms of PsA, and let a healthcare professional know if any of these symptoms occur. They can help refer you to a rheumatologist to determine if you have psoriatic arthritis.

Why trust our experts?



Images used with permission from VisualDx (www.visualdx.com).
References
Alinaghi, F., et al. (2019). Prevalence of psoriatic arthritis in patients with psoriasis: A systematic review and meta-analysis of observational and clinical studies. Journal of the American Academy of Dermatology.
Araujo, E. G., et al. (2020). Enthesitis in psoriatic arthritis (part 1): Pathophysiology. Rheumatology.
Coates, L. C., et al. (2015). Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): A UK multicentre, open-label, randomised controlled trial. The Lancet.
Constantin, M., et al. (2021). Psoriasis beyond the skin: Ophthalmological changes (review). Experimental and Therapeutic Medicine.
Diaz, P., et al. (2022). Characterising axial psoriatic arthritis: Correlation between whole spine MRI abnormalities and clinical, laboratory and radiographic findings. RMD Open.
Dumain, T. (2019). What is sacroiliac (SI) joint pain? The lower back pain you should know about. Creakyjoints.org.
Gwinnutt, J. M., et al. (2022). 2021 EULAR recommendations regarding lifestyle behaviours and work participation to prevent progression of rheumatic and musculoskeletal diseases. Annals of the Rheumatic Diseases.
MedlinePlus. (2014). Psoriatic arthritis.
Ngan, V. (2007). Dactylitis. DermNetNZ.
Pezzolo, E., et al. (2019). The relationship between smoking, psoriasis and psoriatic arthritis. Expert Review of Clinical Immunology.
Scher, J. U., et al. (2019). Preventing psoriatic arthritis: focusing on patients with psoriasis at increased risk of transition. Nature Reviews Rheumatology.
Repinski, K. (2019). What is costochondritis? The alarming arthritis chest pain you might not know about. Creakyjoints.org.
Xie, W., et al. (2020). Modifiable lifestyle and environmental factors associated with onset of psoriatic arthritis in patients with psoriasis: A systematic review and meta-analysis of observational studies. Journal of the American Academy of Dermatology.