Key takeaways:
Milia are tiny white or yellowish bumps that form below the surface of the skin.
Milia are common in infants (milk spots). But they can happen in people of all ages and skin types.
Milia are harmless and usually go away on their own without treatment.
For spots that don’t go away, there are ways to get rid of milia, including exfoliation and medical treatments. These treatments shouldn’t be used on delicate newborn skin.
Milia are tiny, white or yellowish bumps that form beneath the skin surface. Milia (singular term “millum”) are also known as “milk spots.” In fact, up to half of newborns have them. But older children and adults can get them too.
Milia are harmless, but some people may not like the way they look. The good news is that they’re usually temporary and don’t require treatment.
That said, it’s possible to have some stubborn milia that don’t go away. If this is your situation, or you just want to get rid of them quickly, there are treatments that can help get rid of milia for good.
Search and compare options
What causes milia?
It’s not entirely clear what causes milia. One possibility is that they’re tiny cysts that form when old skin cells shed to make room for new ones. Instead of falling off, dead skin cells get trapped underneath new skin. These trapped cells form tiny, hard cysts that are characteristic of milia.
Although extremely common in newborns, milia can occur in anyone. You can see milia in people of all ages, skin types, and racial identities. Some people are more likely to get milia (more on that below). But sometimes, milia can develop for no reason.
Types of milia
Milia are classified either as primary or secondary. The most common type of milia is that seen in infants, a type of primary milia. Other types are less common.
Let’s take a closer look at each type.
Primary milia
Primary milia develop without a known cause. This type includes:
Neonatal milia: This common type is present at birth, usually on or around the nose. But in babies born prematurely, milia may not be seen until later in infancy.
Primary milia of children and adults: These are most common around the eyes, forehead, cheeks, and genitals.
Juvenile milia: These develop as a symptom of a genetic condition (for example, basal cell nevus syndrome). They can be present at birth or seen later in life.
Milia en plaque: This rare form develops when multiple milia are grouped together and form a raised patch of skin. The patch can be the width of a quarter or larger. It’s usually on the eyelid, cheek, or behind the ear.
Multiple eruptive milia: In this rare type, many milia appear over a few weeks to months. They’re usually on the face, upper arms, and abdomen.
Bumps on your face? From cysts to moles, learn about the most common bumps on your face that aren’t acne (with pictures).
Sebaceous cysts: Read about these common cysts and learn how to identify and get rid of them (with photos).
Could it be cancer? Some bumps on the face are cancer. Learn what different types of skin cancer look like (with pictures).
Secondary milia
Secondary milia develop as a result of an underlying cause or condition. This type includes:
Trauma-associated: This can happen following damage to the skin from injuries or procedures, like with dermabrasion, burns, or chronic sun exposure.
Disease-associated milia: This type of milia occurs from rare blistering skin diseases, like epidermolysis bullosa or bullous pemphigoid.
Medication-associated: This rare form typically appears with chronic use of certain medicated creams, like steroids or fluorouracil.
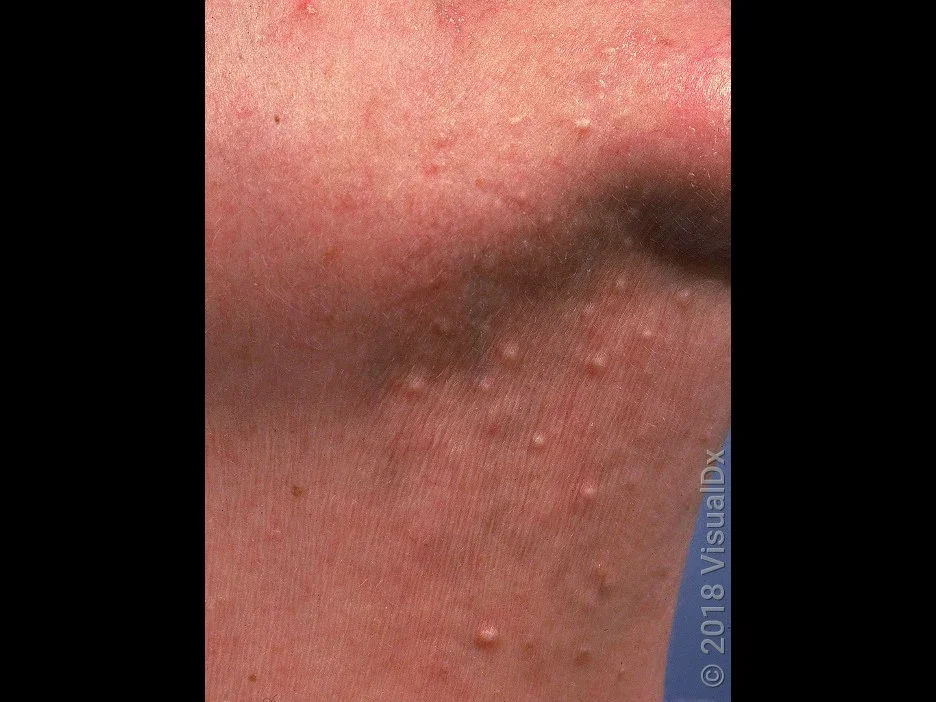
Pictures of milia
Milia are most common on the face, especially around the eyes and cheeks. But they can happen anywhere on the body, including the:
Scalp
Chest
Arms
Legs
Genitals
Read more like this
Explore these related articles, suggested for readers like you.
Here are some pictures of milia bumps on different locations and in different skin tones.



How do you get rid of milia?
Newborn milia don’t need treatment because they go away on their own within a month. We’ll say it again so you don’t miss it: Newborn milia don’t need treatment.
Other types of milia usually go away on their own within a few months. In both situations, milia usually heal without scarring.
But sometimes milia don’t resolve on their own and need treatment to go away. In these cases, here are some at-home and medical treatments for milia that may help. These treatments aren’t to be used on delicate newborn skin.
1. Exfoliate
In older children and adults, exfoliating can help treat and prevent milia by removing dead skin cells. It can take a few weeks before you see an improvement. Here are some tips for exfoliating at home:
Pick the best exfoliator for your skin type. For sensitive skin, try a mild chemical exfoliator (like low-dose lactic acid). For oilier skin, try a physical exfoliator (like a scrub wash) or a higher-strength chemical exfoliator.
Be gentle. Apply the exfoliator gently for about 30 seconds without too much pressure.
Use a moisturizer. Apply a moisturizer right after exfoliating.
Don’t overdo it. How much you can exfoliate depends on your skin type and the strength of the exfoliator. Stronger exfoliators should be used less often. Oily skin can be exfoliated 2 or 3 times a week, while sensitive skin may be once a week or less.
2. Try a retinoid
Retinoids are medications used to treat acne and other skin concerns. They work by exfoliating the skin and unclogging pores. They can also work as a treatment for milia, but only in adults. If you have milia, here are some tips to using a retinoid:
Stronger, prescription-strength retinoids work better. Ask your primary care provider for a prescription, or use 0.1% Differin, which is available over the counter (OTC).
Start low, go slow. All retinoids can irritate your skin. Start by using a tiny amount on the affected area every other night. Increase to nightly if your skin isn’t getting red or irritated.
Be patient. It may take weeks or longer to notice an improvement.
3. Explore in-office procedures
Several medical procedures can get rid of milia. Sometimes, just one treatment is all that’s needed. It’s important to go to a dermatologist or other professional trained in the procedure. Side effects like scarring or hyperpigmentation are more likely if the procedure isn’t done correctly. Keep in mind that these types of treatments aren’t usually covered by insurance.
Here are some types of medical procedures that may treat milia:
Cryotherapy: Liquid nitrogen is applied to the skin to freeze and remove milia.
Surgical removal: A small incision is made with a tiny needle or blade tip to remove the milia.
Curettage: A tiny blade is used to scrape off milia.
Laser resurfacing: A laser is used to break down the milia.
Chemical peels: High-strength exfoliants are used to remove the top dead layer of skin cells.
Dermabrasion: A handheld device is used to exfoliate the top layer of skin.
4. Don’t pick!
Remember, avoid picking at or squeezing milia. This can lead to scarring or infection. For this reason, dermatologists don’t recommend trying to remove milia at home with needles or using any milia removal tools.
How to prevent milia
There’s no way to prevent milia. But you can reduce your risk of developing it by following a skin care routine.
A good skin care routine is important for treating and preventing milia. This will help get rid of debris and dead skin cells and keep your skin healthy. Here are some tips for what that looks like in practice:
Cleanse daily. Use a mild cleanser twice a day and after sweating.
Moisturize regularly. After cleansing your face, use a gentle moisturizer to hydrate and protect your skin.
Choose your products carefully. Limit or avoid heavy oil-based products, and keep topical steroid use to a minimum.
Apply sunscreen. Use broad-spectrum sunscreen on your face every day. This will protect you against skin cancer and help prevent milia from forming.
Frequently asked questions
No. In fact, the opposite is true. Milia are most common in newborns, in the first few weeks of life. There are other reasons why people may have milia, at any stage of life. But milia in older people is less common.
The fastest way to remove milia is for your dermatologist to remove them in the office with a procedure (like surgical removal). The next best option is to exfoliate your skin. This can be done with chemical exfoliators (like salicylic acid) or topical retinoids (like tretinoin).
No. Milia aren’t caused by a vitamin deficiency. If you’re worried that you may have a vitamin deficiency, talk to your primary care provider before starting any type of supplement.
No. In fact, the opposite is true. Milia are most common in newborns, in the first few weeks of life. There are other reasons why people may have milia, at any stage of life. But milia in older people is less common.
The fastest way to remove milia is for your dermatologist to remove them in the office with a procedure (like surgical removal). The next best option is to exfoliate your skin. This can be done with chemical exfoliators (like salicylic acid) or topical retinoids (like tretinoin).
No. Milia aren’t caused by a vitamin deficiency. If you’re worried that you may have a vitamin deficiency, talk to your primary care provider before starting any type of supplement.
The bottom line
Milia are most common in newborns. But they can occur at any age and with any skin type. But rest assured, milia aren’t dangerous, and treatment isn’t usually needed. Milia tend to resolve on their own within a few weeks to months. If you have milia that aren’t clearing up or that are getting worse, talk to a healthcare professional. They can work with you on the next steps for treatment and prevention.

Why trust our experts?



Images used with permission from VisualDx (www.visualdx.com).
References
American Academy of Dermatology Association. (n.d.). Epidermolysis bullosa: Overview.
American Academy of Dermatology Association. (n.d.). Face washing 101.
American Academy of Dermatology Association. (n.d.). How to safely exfoliate at home.
American Academy of Dermatology Association. (n.d.). Microdermabrasion: FAQs.
American Society for Dermatologic Surgery. (n.d.). Dermabrasion.
Connelly, T. (2008). Eruptive milia and rapid response to topical tretinoin. Archives of Dermatology.
Gallardo Avila, P. P., et al. (2023). Milia. StatPearls.
Gupta, M., et al. (2009). Milium. DermNet.
Oakley, A., et al. (2021). Basal cell naevus syndrome. DermNet.


















