Key takeaways:
A heart attack and cardiac arrest are both serious medical emergencies, but they’re different conditions.
A heart attack can sometimes lead to a cardiac arrest, but it’s not the only cause.
Treatment for a heart attack depends on the type of heart attack. But treatment for cardiac arrest is always cardiopulmonary resuscitation, or CPR.
A heart attack and a cardiac arrest are both medical emergencies. Their names might sound similar, but they’re not the same. Someone can have a heart attack without cardiac arrest, and someone else may have cardiac arrest without having a heart attack. Let’s review each condition, which symptoms to look for, and what you should do if you think someone is having a heart attack or cardiac arrest.
What is the difference between a heart attack and a cardiac arrest?
Is cardiac arrest the same as a heart attack? No, they are different conditions.
Heart attack
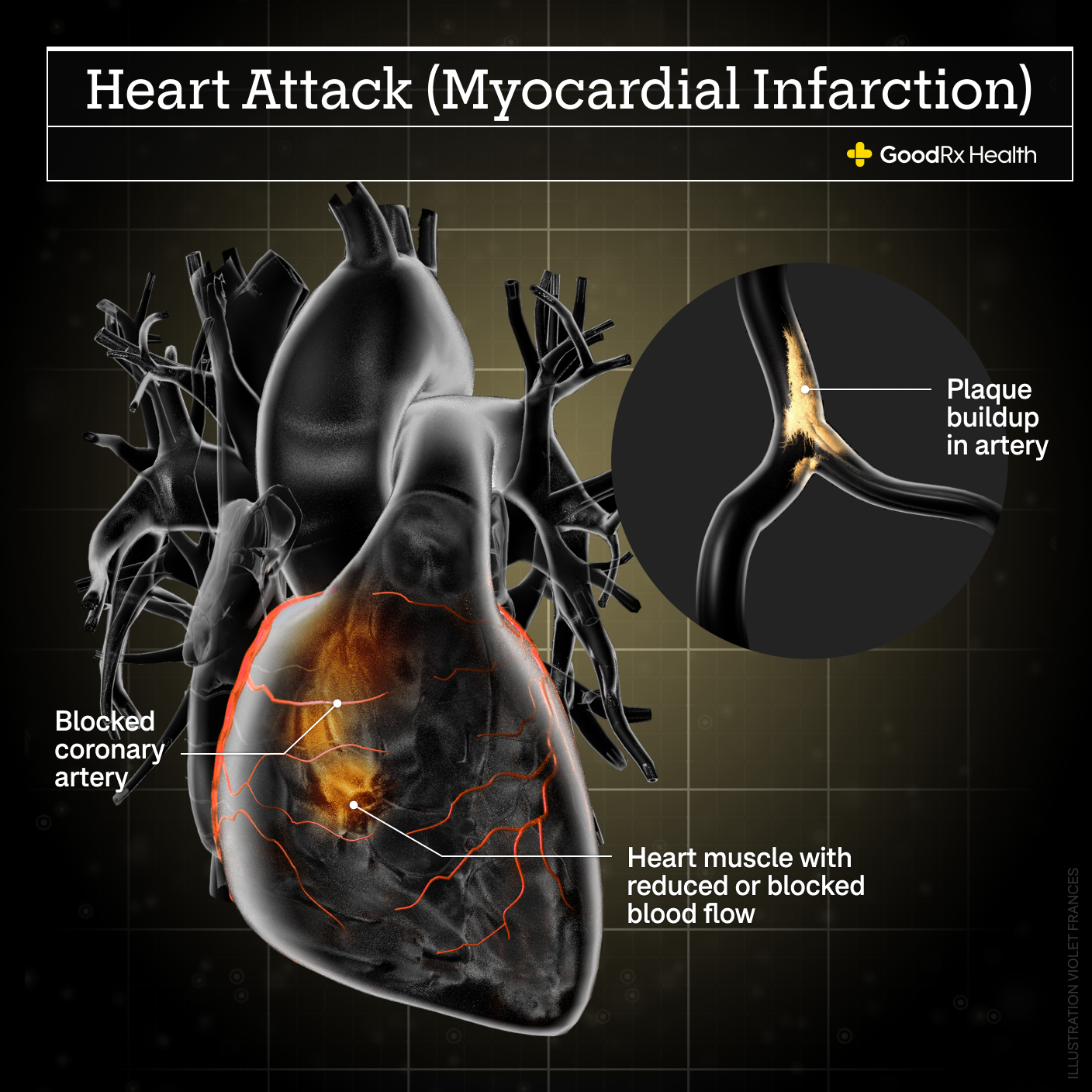
A heart attack happens when your heart muscle can’t get enough blood. This can happen due to:
A blockage in one of the arteries that supply blood to the heart muscle
A spasm in one of the blood vessels
Increased stress on the heart
Symptoms of a heart attack include:
Chest pain
Pain in the left side of the jaw or left arm
Shortness of breath
Nausea
Cardiac arrest
A cardiac arrest happens when your heart suddenly stops pumping blood normally. This can happen because:
The heart stops beating
The heart develops an abnormal rhythm that keeps it from effectively pumping blood
Some people who have a cardiac arrest have a history of heart disease, but some don’t. Symptoms of a cardiac arrest are:
Loss of consciousness
Loss of pulse
Which is more dangerous, a heart attack or a cardiac arrest?
A cardiac arrest is more dangerous than a heart attack. Without treatment, it can be fatal within minutes. Up to 80% of people who have a cardiac arrest outside of a hospital die before reaching the hospital. Even with immediate treatment, the risks for brain damage after a cardiac arrest are high.
A heart attack can sometimes result in death, but it’s less likely to cause death than a cardiac arrest. Sometimes, people who have risk factors for heart disease may have brief episodes of reduced blood flow to the heart in the days or weeks before having a heart attack.
Unlike during a cardiac arrest, the heart usually still pumps blood around the body during a heart attack. Even when a heart attack happens suddenly, treatment within hours, rather than minutes, can still be lifesaving.
It’s important to note that while a heart attack and a cardiac arrest are different, a heart attack may increase the risk of having a cardiac arrest.
What causes a cardiac arrest?
Cardiac arrests are often caused by heart disease, but not always. Other heart problems can increase your risk of cardiac arrest, including:
Heart attack
A history of arrhythmia (irregular heart rhythm)
Cardiac arrests can also be caused by:
Electrolyte imbalances in the blood
Low blood oxygen levels
Low body temperature
Blood clots in the lungs or heart
Trauma or accidents
Certain drugs or toxins
How can you tell whether someone is having a heart attack or a cardiac arrest?
It can be difficult to tell whether someone is having a heart attack. One reason for this is that the symptoms of a heart attack can be different for different people. Another reason is that other conditions — like a panic attack, heartburn, or asthma attack — can sometimes cause some of the same symptoms.
There are some symptoms that make it likely that someone is having a heart attack, especially if they have a history of heart disease, like:
Chest pain or chest pressure
Shortness of breath
Pain in the jaw, neck, arms, or back
Nausea and vomiting
Lightheadedness
A cardiac arrest is much easier to spot. Symptoms of a cardiac arrest include loss of consciousness, difficulty breathing, and loss of pulse.
Someone who has a cardiac arrest may:
Appear very pale
Not be able to respond to voice or touch
Have difficulty breathing
Have a weak pulse or no pulse at all
If a person with a cardiac arrest is hooked up to a heart monitor, the heart rhythm may look abnormal or there could be no rhythm at all — just a flat line. This means that the electrical activity in the heart is abnormal or there’s no electrical activity at all.
What are the risk factors for a cardiac arrest?
The risk factors for cardiac arrest are similar to the risk factors for heart disease or a heart attack. There are major and minor risk factors, and some risk factors are related to lifestyle. Risk factors that you may be able to change are known as modifiable risk factors.
Major risk factors
The major risk factors of cardiac arrest include:
Increasing age
Being born male
Family history of heart disease, heart attack, or sudden cardiac death
Modifiable risk factors
Modifiable risk factors include:
Smoking
High cholesterol
High blood pressure
Type 2 diabetes
Minor risk factors
Minor risk factors include:
Stress level
Alcohol use
Poor diet and nutrition
What is the treatment for a heart attack or cardiac arrest?
Both heart attacks and cardiac arrest are emergencies that need immediate medical care.
The treatment for a cardiac arrest is cardiopulmonary resuscitation, or CPR. CPR involves doing chest compressions to help the heart pump blood through the body and giving breaths to help deliver oxygen to the lungs.
Another important part of treating a cardiac arrest is using an automated external defibrillator, or AED. An AED is a simple-to-use machine that can analyze the heart’s rhythm and deliver an electric shock, if necessary, to treat an abnormal rhythm.
There are many different treatments for a heart attack. Often, treatment involves a combination of medications that:
Thin the blood
Slow down the heart rate
Decrease the blood pressure
Treat pain
Depending on the type of heart attack, a procedure known as a cardiac catheterization to help improve blood flow to the heart may be necessary. Some people may only need a cardiac catheterization. Others may need an emergency heart surgery known as coronary artery bypass graft (CABG).
What can you do if you think someone may be having a heart attack or cardiac arrest?
If you think someone may be having a heart attack or cardiac arrest, it’s important to act right away. The first thing to do is to make sure the scene is safe and then to check whether the person is breathing and has a pulse. If you see that someone isn’t breathing or doesn’t have a pulse, call for help immediately and begin chest compressions. If you’re trained in CPR, ask for an AED or grab the nearest one. A lot of public places have AEDs easily available. Even if you aren’t trained in CPR, calling for help and starting chest compressions until help arrives is very important and can make a big difference.
Starting CPR as quickly as possible is extremely important. If CPR isn’t started within minutes, cardiac arrest is much more likely to be fatal.
If someone is having a heart attack, then they may be breathing, have a pulse, and be able to respond to you. In this case, you should stay with the person and call 911, even if you aren’t sure whether the person is actually having a heart attack. It’s also important to get as much health information from the person as you can. Having the person’s medical information can help emergency responders better care for the person, especially if they aren’t able to talk when help arrives.
Is cardiac arrest fatal?
Cardiac arrest isn’t always fatal. Bystander training in CPR coupled with the availability and use of AEDs mean that more people are surviving sudden cardiac arrest. In the past, cardiac arrest was almost always fatal. Now, about 20% of people survive and leave the hospital.
Unfortunately, about 350,000 people die from sudden cardiac arrest every year in the U.S. The key to survival is starting CPR or using an AED within minutes of the arrest.
Is cardiac arrest painful?
Loss of consciousness is usually the first and only sign of sudden cardiac arrest. Sometimes people may experience symptoms like chest pain or chest fullness within the hour before cardiac arrest. Other vague symptoms right before sudden cardiac arrest include:
Racing heart
Nausea
Vomiting
Dizziness
Lightheadedness
Most people don’t have any symptoms before sudden cardiac arrest. But if a person receives CPR for cardiac arrest, they may have muscle and rib pain during their recovery period.
The bottom line
A heart attack and a cardiac arrest are both serious cardiovascular emergencies, but they aren’t the same. Some of the risk factors for both a heart attack and a cardiac arrest are similar, but the symptoms and treatments are different. A cardiac arrest is more worrisome because it’s more likely to be fatal. Immediate treatment is very important for both a heart attack and a cardiac arrest.

Why trust our experts?



References
American Heart Association. (2022). Heart attack and sudden cardiac arrest differences.
American Heart Association. (2022). Understand your risks to prevent a heart attack.
American Heart Association. (2023). Emergency treatment of cardiac arrest.
American Heart Association. (2023). Heart attack treatment.
Centers for Disease Control and Prevention. (2024). About cardiac arrest.
Centers for Disease Control and Prevention. (2024). About heart attack symptoms, risk, and recovery.
MedlinePlus. (2017). Coronary artery bypass surgery.
MedlinePlus. (2023). Sudden cardiac arrest.
National Heart, Lung, and Blood Institute. (2023). Out-of-hospital cardiac arrest: NHLBI studies tackle deadly public health problem.
Patel , K., et al. (2023). Cardiac arrest. StatPearls.












