Key takeaways:
The cause of Legionella disease is Legionella bacteria, which lives in water and soil.
Legionella doesn’t always make people sick, but it can cause pneumonia and Pontiac fever, a mild illness.
Antibiotics can treat Legionnaires’ disease.
Legionella are bacteria that live around us in water and soil. Usually they aren’t harmful, but in some cases Legionella can make us sick. When Legionella infects the lungs it causes Legionnaires’ disease, a type of pneumonia. It can also cause Pontiac fever, a milder illness that usually goes away on its own. While pneumonia can sound scary, the good news is that you can treat Legionella disease with antibiotics.
Keep reading to find out more about the spread, diagnosis, and treatment of Legionella infection.
What is Legionella bacteria, and how does it spread?
Legionella bacteria include many species that live in water and soil. Some species, like Legionella longbeachae, are in soil, including potting mixes. Another species, Legionella pneumophila, lives in water. This species is the most common cause of illness in humans.
Legionella live in freshwater, like lakes and streams. But infections are more likely to occur from human-made water sources, including:
Hot tubs
Industrial air conditioning systems
Large plumbing systems
Hot water tanks
Fountains and water features
Legionella can grow and multiply in these water sources, making it easier to cause infection. Testing a water source is the only way to know that it’s contaminated with Legionella. Infection starts after someone inhales contaminated water droplets or soil particles in the air. It can also happen when someone who has difficulty swallowing accidentally inhales contaminated water or ice (aspiration).
How do you get Legionnaires' disease?
Legionnaires’ disease happens when Legionella bacteria infect the lungs. The name of the disease comes from a 1976 outbreak at an American Legion in Philadelphia, Pennsylvania. Outbreaks can occur when groups of people come into contact with the bacteria in contaminated water and get infected.
In 2018, there were about 10,000 cases of Legionnaires’ disease in the U.S. Single cases of Legionnaires’ disease can occur in individuals, and they’re more common than outbreaks.
Certain people are at higher risk for Legionnaires’ disease, including:
Adults over age 50
People with decreased immune systems
People who smoke or used to smoke
People with chronic illnesses (like diabetes and kidney or lung disease) or cancer
Considering the bacteria is always around us, infection with Legionella is rare. This means that even if you’re exposed to Legionella, it won’t always make you sick.
What are the symptoms of Legionella disease?
The symptoms of Legionnaires’ disease are similar to those in other types of pneumonia, including:
Fever
Fatigue
Chest discomfort
Cough
Shortness of breath
In Legionnaires’ disease these symptoms start 2 to 10 days after you’re exposed to the bacteria.
Legionella can also cause Pontiac fever, but it’s milder than Legionnaires’ disease. Symptoms usually start 1 to 2 days after exposure and include:
Fever
Headache
Body aches
Nausea and vomiting
Diarrhea
How do you diagnose Legionella infections?
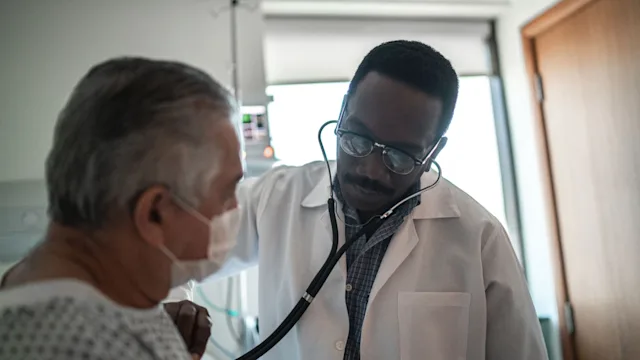
Your provider may suspect Legionnaires’ disease based on your symptoms and physical examination. With pneumonia, your lungs sound abnormal when your healthcare provider listens with a stethoscope. A chest X-ray can confirm the diagnosis of pneumonia.
Since Legionnaires’ disease acts like other types of pneumonia, testing can identify Legionella as the specific cause. Lab testing on a sample of sputum (phlegm) or urine can diagnose Legionnaires’ disease. Testing is most important when pneumonia is severe because it helps guide treatment.
You don’t need testing for Pontiac Fever. This is because it's a mild illness that goes away on its own — without treatment — within about 1 week.
How do you treat Legionnaires' disease?
You can treat Legionnaires’ disease with antibiotics. Once a healthcare provider diagnoses pneumonia, they’ll recommend you start taking antibiotics right away. This is a common treatment for bacterial causes, including Legionella. You can start antibiotics before Legionella testing comes back.
Once testing confirms Legionella, your provider may recommend treatment with fluoroquinolones or macrolides if you hadn’t already started taking these. These are the preferred classes of antibiotics for this type of pneumonia. Specifically, antibiotics that treat Legionnaires’ disease include Levofloxacin (Levaquin), a fluoroquinolone, and azithromycin (Zithromax), a macrolide.
If you need treatment in the hospital for Legionnaires’ disease, you’ll likely get antibiotics through an intravenous (IV) infusion. Once your symptoms improve, you’ll switch from IV antibiotics to oral antibiotics (in pill form). Treatment lasts at least 5 days, but some cases need longer treatments.
How serious is Legionella disease?
Legionella disease can range from mild to severe. People with underlying medical conditions are more likely to have severe Legionella disease. Some people may need treatment in the hospital. About 1 in 10 people with Legionnaires’ disease will die from it.
There’s no mistaking that Legionnaires’ disease presents a serious health risk. But it’s important to remember that antibiotics can treat most cases of Legionnaires’ disease. Starting antibiotics early in the illness improves outcomes. So if you notice symptoms, be sure to connect with your healthcare provider right away.
Is Legionella disease contagious?
According to experts, Legionella disease is very unlikely to spread between people. This means to get it you must be exposed to water or soil with Legionella bacteria. There’s one known probable case of Legionella disease that spread from one person to another. But this is very unusual.
The bottom line
The cause of Legionella disease is Legionella bacteria that live around us in water and soil. Most of the time Legionella doesn’t make us sick. But exposure can lead to outbreaks of Legionnaires’ disease — a pneumonia that can be severe in some people. It can also cause Pontiac fever, a mild illness. The good news is antibiotics are effective against Legionnaires’ disease, and Pontiac fever tends to go away on its own.

Why trust our experts?


References
Correia A. M., et al. (2016). Probable person-to-person transmission of Legionnaires’ disease. New England Journal of Medicine.
Centers for Disease Control and Prevention. (2021). About the disease.
Centers for Disease Control and Prevention. (2021). Causes, how it spreads, and people at increased risk.
Centers for Disease Control and Prevention. (2021). Fast facts.
Metlay J. P., et al. (2019). Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine.
World Health Organization. (2018). Legionellosis.