Key takeaways:
Scrambler therapy is a noninvasive approach to treating chronic pain and pain from cancer.
The treatment uses a device that sends electrical impulses through your skin to change the way you perceive pain.
Scrambler therapy may reduce symptoms of pain conditions, including chronic pain, cancer-related pain, and diabetic neuropathy.
The treatment takes about 1 to 2 weeks and is not usually covered by insurance.
Scrambler therapy is a type of noninvasive treatment for chronic pain. It uses a device that delivers electrical impulses to your nerves to change the way you perceive pain signals.
People with chronic pain may not get relief from pain medications alone, and often other treatments like behavioral strategies don’t offer enough pain relief. So using alternative approaches to pain management can be an important part of treatment.
One promising approach is to target pain signals directly with electrical stimulation devices like scrambler therapy. In fact, these types of devices are also used to help prevent and reduce migraines.
Search and compare options
Read on to learn how scrambler therapy works and if you should consider it to help treat your pain.
What is scrambler therapy?
Scrambler therapy uses a device to treat chronic pain and other types of pain. It’s based on a theory that you can retrain your brain to interpret pain signals differently.
The device sends electrical impulses through the skin into nerve endings. The stimulation targets pain signals and reorganizes or “scrambles” them. Your brain then may interpret the signals as nonpainful messages.
Scrambler therapy is performed in a medical office or pain clinic by a professional trained in the procedure. Though it has similarities to transcutaneous electrical nerve stimulation (TENS) units, it cannot be done at home.
What does scrambler therapy feel like?
During the procedure, electrodes, like those used for an electrocardiogram (EKG), are placed near the areas where you have pain. They are not placed directly where you have pain.
When the device is turned on, electrical impulses penetrate through the skin to stimulate nerve fibers. The treatment may be a little uncomfortable. Some people report that it feels like little bee stings at first. The intensity of the stimulation can be adjusted if it’s too uncomfortable.
How to reduce opioid pain relievers: Learn about nonopioid pain medications and alternative treatments for pain.
Getting relief may depend on how you advocate for yourself. Here’s how to talk with your healthcare team about your pain.
Learning to manage pain can improve your quality of life. Explore these mental health therapies that can help.
The feeling will change to a more comfortable humming or vibrating sensation in the nerve. A treatment lasts 30 to 45 minutes. By the end of the session, you may feel less or no pain.
Usually therapy consists of daily treatments for 1 to 2 weeks. On the first day, your pain relief may only last an hour or so, but each day, the pain relief lasts longer until the pain doesn’t return at all.
Pain relief is supposed to last for weeks to months after treatment is stopped. When pain starts to return, one to two booster treatments may provide ongoing relief.
- HycetHydrocodone/Acetaminophen
- XodolHydrocodone/Acetaminophen
- IbuprofenGeneric Motrin
What conditions does scrambler therapy help treat?
Scrambler therapy may help with several types of pain. You may experience short-term pain relief but no one knows how long that relief will last. Studies only have evidence of 2 to 4 weeks of relief from treatment. Pain is complex and has many different causes, and people react differently to treatments.
Studies have looked at people with different types of pain — chronic pain, pain related to cancer, and neuropathic pain (related to nerve damage).
Chronic pain
Chronic pain is defined as pain that lasts longer than 3 to 6 months. One study found that scrambler therapy reduced chronic pain symptoms by about 50%. The trial found that the number of people who experienced severe pain dropped from 76 before treatment to 16 after treatment. But participants were only followed for 2 weeks, so it’s not clear if they experienced pain relief after that time.
In a review of studies, researchers found that people who used scrambler therapy took less pain medication (such as opioids). That can lower the risk of side effects from these treatments.
Cancer pain
Pain affects 50% to 70% of people with cancer. Pain can be a symptom of cancer, and it can be a side effect of cancer treatments. For example, chemotherapy can cause nerve damage that leads to pain. That’s called chemotherapy-induced peripheral neuropathy.
The research on using scrambler therapy for cancer pain is still limited, but the studies tend to show that it may help reduce pain.
A small study of people with chemotherapy-induced peripheral neuropathy found that scrambler therapy reduced their pain, numbness, and tingling.
Neuropathic pain
Neuropathic pain is usually caused by injury or damage to a nerve. Diabetes is one common cause of neuropathic pain.
One study found that scrambler therapy offered significant short-term pain relief in people being treated for severe neuropathic pain. And another small study found it reduced severe pain in people with diabetic neuropathy for about a month after treatment, but they didn’t have longer-term relief.
How much does scrambler therapy cost?
Scrambler therapy received FDA clearance in 2009. But it’s considered investigational because there’s no evidence showing that it works consistently for most people or that it provides lasting pain relief. That means that Medicare and most insurers don’t cover this therapy.
The cost of the procedure can range from $200 to $300, but it may be as high as $500 per session. The cost varies by your location and the specific center. Treatment usually consists of 10 to 12 sessions over 2 weeks.
Who should not use scrambler therapy?
Scrambler therapy may be safe for most people. But it’s not recommended for people with certain health conditions. The professional who’s treating you will ask you about your medical history to make sure it’s safe for you to get the treatment. People with these conditions may not be able to use scrambler therapy:
Having a pacemaker or automatic defibrillator
Having an aneurysm clip, vena cava clips, or skull plates
Being pregnant or breastfeeding
Having a history of epilepsy or brain damage
Having severe arrhythmia or severe heart disease
Having skin irritation or wounds near the area that would be treated
Having an implanted drug delivery system
What are the best alternatives to scrambler therapy?
Another treatment that uses electrical current to treat pain is called TENS, or transcutaneous electrical nerve stimulation. TENS can be done in a physical therapy or pain clinic or you can buy a TENS machine to use at home. (You can buy a TENS machine in stores or online. They cost between $30 to $70.)
Although both scrambler therapy and TENS use electrical nerve stimulation, they target different nerves. TENS units use electrical impulses to block pain signals or distract the brain. Scrambler therapy uses electrical impulses to trick the brain into thinking the impulses are not painful.
One review of the research found that TENS may help provide immediate pain relief for musculoskeletal pain like arthritis. But other reviews have found that there’s a lack of good studies showing it’s effective.
Frequently asked questions
Studies show that scrambler therapy may provide pain relief for people with chronic pain. But the evidence hasn’t shown that it provides long-term pain relief. The effectiveness varies depending on what you’re treating, and everyone responds differently to pain treatments. One of the most studied uses of scrambler therapy is on nerve pain due to chemotherapy.
No, a specialized machine is needed for scrambler therapy. The machines are not available for home use. Scrambler therapy is delivered by a trained professional in a medical setting. Also, it’s typically given as a single course of treatment over 2 weeks, not something you continue to do on a daily or weekly basis.
Insurance typically doesn’t cover scrambler therapy. You’ll have to pay out of pocket for your sessions. Pricing differs depending on where you have it done, and the number of sessions needed.
Studies show that scrambler therapy may provide pain relief for people with chronic pain. But the evidence hasn’t shown that it provides long-term pain relief. The effectiveness varies depending on what you’re treating, and everyone responds differently to pain treatments. One of the most studied uses of scrambler therapy is on nerve pain due to chemotherapy.
No, a specialized machine is needed for scrambler therapy. The machines are not available for home use. Scrambler therapy is delivered by a trained professional in a medical setting. Also, it’s typically given as a single course of treatment over 2 weeks, not something you continue to do on a daily or weekly basis.
Insurance typically doesn’t cover scrambler therapy. You’ll have to pay out of pocket for your sessions. Pricing differs depending on where you have it done, and the number of sessions needed.
The bottom line
Scrambler therapy is a promising treatment for certain types of ongoing pain. It works by sending electrical impulses through your skin to scramble nerve messages. This can retrain your brain to interpret the messages as nonpainful. Scrambler therapy can be used along with other treatments, and may help reduce the need for pain medications.

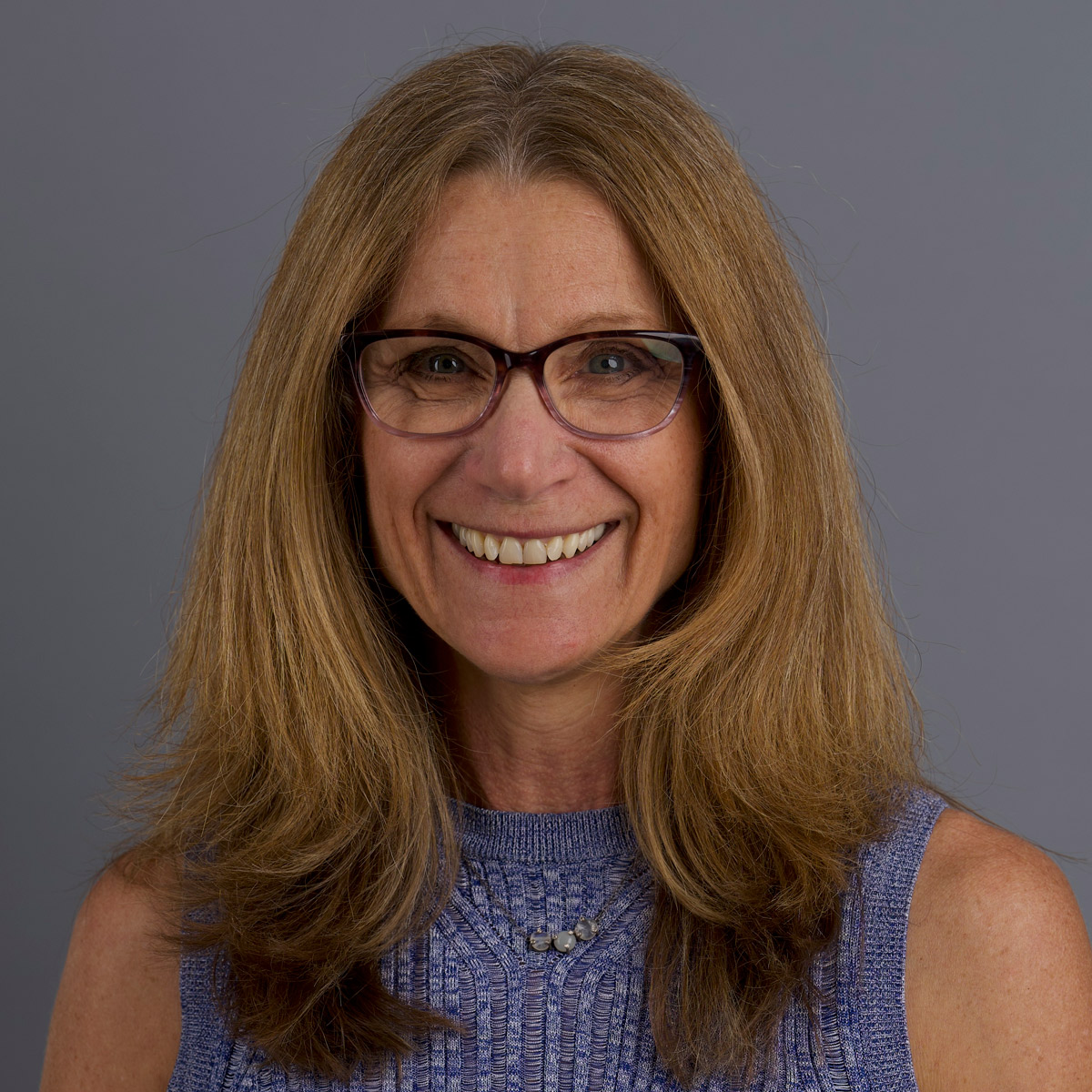
Why trust our experts?


References
Calmare. (n.d.). Who it’s for.
Chung, M., et al. (2024). The impact of scrambler therapy on pain and quality of life for chemotherapy-induced peripheral neuropathy: A pilot study. Pain Practice.
Dydyk, A. M., et al. (2024). Chronic pain. StatPearls.
Jin, Y., et al. (2022). Efficacy of scrambler therapy for management of chronic pain: a meta-analysis of randomized controlled trials. Pain Physician.
Johnson, M., et al. (2007). Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: A meta-analysis of randomized controlled trials.
Kashyap, K., et al. (2020). Evidence for the efficacy of scrambler therapy for cancer pain: A systematic review. Pain Physician.
Majithia, N., et al. (2016). Scrambler therapy for the management of chronic pain. Supportive Care in Cancer.
Marineo, G. (2019). Inside the scrambler therapy, a noninvasive treatment of chronic neuropathic and cancer pain: From the gate control theory to the active principle of information. Integrative Cancer Therapies.
Max Wellness Pain Relief. (n.d.). Announcement: Updated pricing.
Non-Surgical Spine Center. (n.d.). Life changing scrambler therapy.
Paley, C. M., et al. (2021). Does TENS reduce the intensity of acute and chronic pain? A comprehensive appraisal of the characteristics and outcomes of 169 reviews and 49 meta-analyses. Medicina.
Ricci, M., et al. (2019). Scrambler therapy: What's new after 15 years? The results from 219 patients treated for chronic pain. Medicine.
Smith, T., et al. (n.d.). Scrambler therapy for treating neuropathic pain. The Foundation for Peripheral Neuropathy.
University of California, Los Angeles. (n.d.). Scrambler therapy for chronic pain.
Wang, E. J., et al. (2023). Safety of scrambler therapy: A systematic review of complications and adverse effects. Pain Medicine.
Yoo, S. H., et al. (2023). Efficacy of scrambler therapy in patients with painful diabetic peripheral neuropathy: A single-arm, prospective, pilot study. Medicine.