Mirena
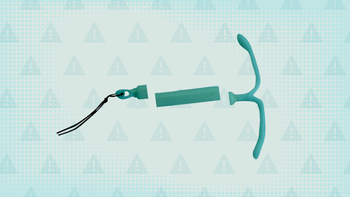
Mirena (levonorgestrel) is a progestin intrauterine device (IUD). It's approved for females of reproductive age to prevent pregnancy for up to 8 years. It can also help relieve heavy menstrual periods for up to 5 years. Mirena IUD (levonorgestrel) is inserted into the uterus by a provider in their office. Some of the more common side effects of Mirena IUD (levonorgestrel) include changes to menstrual bleeding and pelvic pain. Rarely, it can also cause some weight gain.

What is Mirena IUD (levonorgestrel)?
What is Mirena IUD (levonorgestrel) used for?
Prevent pregnancy for up to 8 years
Relieve heavy menstrual periods for up to 5 years
How Mirena IUD (levonorgestrel) works
Mirena IUD (levonorgestrel) is a small device placed in the uterus that slowly releases a progestin hormone called levonorgestrel. This hormone prevents pregnancy by stopping your ovaries from releasing an egg. Levonorgestrel also makes it difficult for sperm to enter the uterus and for a fertilized egg to implant in the uterus. Mirena IUD (levonorgestrel) works to treat heavy periods by thinning the lining of your uterus.
Drug Facts
More on Mirena IUD (levonorgestrel) essentials

What are the side effects of Mirena IUD (levonorgestrel)?
Common Side Effects
- Abnormal uterine bleeding (up to 32%)
- Stomach or pelvic pain (23%)
- No menstrual bleeding (18%)
- Headaches or migraines (16%)
- More vaginal discharge than usual (15%)
- Vaginal irritation (11%)
Other Side Effects
- Breast pain
- Ovarian cyst
- Menstrual cramps
- Back pain
- Acne
- Depression
- Hair loss
- Facial hair growth
- Expulsion (the device comes out on its own)
- Weight gain
- Nausea
Serious Side Effects
- Ectopic pregnancy: severe, unexplainable pelvic pain along with unusual vaginal bleeding
- Severe infection: fever, chills, confusion, fatigue
Source: DailyMed
More on Mirena IUD (levonorgestrel) side effects
The following side effects have also been reported
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor or nurse immediately if any of the following side effects occur:
More common
Absent, missed, or irregular menstrual periods
longer or heavier menstrual periods
mild bloating
stomach or pelvic pain
stopping of menstrual bleeding
unusually heavy or unexpected menstrual bleeding
uterine bleeding between menstrual periods
vaginal bleeding or spotting
Less common
Blurred vision
cramps
dizziness
headache
itching of the vagina or genital area
nervousness
pain during sexual intercourse
pale skin
pounding in the ears
slow or fast heartbeat
swelling
thick, white vaginal discharge with mild or no odor
trouble breathing
unusual bleeding or bruising
unusual tiredness or weakness
white or brownish vaginal discharge
Rare
Chills
confusion
dizziness, lightheadedness, fainting
fast heartbeat
fast, weak pulse
pale, cold, clammy skin
rapid, shallow breathing
sudden increase in stomach or shoulder pain
sweating
unusual or large amount of vaginal bleeding
Incidence not known
Clear or bloody discharge from the nipple
dimpling of the breast skin
dull or aching stomach pain
foul-smelling vaginal discharge
increased blood pressure
increased urge to urinate
inverted nipple
large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
lump in the breast or under the arm
pain during urination
persistent crusting or scaling of the nipple
redness or swelling of the breast
severe stomach pain or cramping
sharp pain on insertion
shivering fever
sores on the skin of the breast that does not heal
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
Back pain
breast tenderness or pain
decreased interest in sexual intercourse
full or bloated feeling
hives or welts, itching, or rash
increased hair growth, especially on the face
increased weight
loss in sexual ability, desire, drive, or performance
pressure in the stomach
redness of the skin
skin rash, encrusted, scaly, and oozing
swelling of the stomach area
thinning of the hair
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.

Pros and cons of Mirena IUD (levonorgestrel)

Pros
Work better than (works better) oral birth control pills to prevent pregnancy
Can be used while breastfeeding
Can be inserted in your provider's office within a few minutes and without any kind of sedation (medication to put you asleep)
Helps relieve heavy menstrual periods for up to 5 years

Cons
Can raise your risk of an ectopic pregnancy
Breakthrough bleeding and irregular cycles are common side effects
Not safe to use if you have liver problems or have ever had breast, uterine, or cervical cancer
Can't be used if you have uterine fibroids, are prone to pelvic infections, or have pelvic inflammatory disease (PID)

Pharmacist tips for Mirena IUD (levonorgestrel)

You might feel some pain, dizziness, or have some light vaginal bleeding after the Mirena IUD (levonorgestrel) has been placed, but it should be temporary. If these symptoms don't lessen after a few days, tell your provider.
After the Mirena IUD (levonorgestrel) has been placed, there will be 2 thin threads hanging inside the vagina. Your provider might recommend that you check for these threads once a month with a clean finger. Never tug or pull on the threads when you're checking for them. If you can't feel them, call your provider right away because it might be a sign that Mirena IUD (levonorgestrel) isn't positioned properly.
The Mirena IUD (levonorgestrel) can affect your menstrual cycle and menstrual bleeding. It's possible you might even have no period while using this device. Call your provider if this is concerning to you or if your bleeding becomes very heavy.
The Mirena IUD (levonorgestrel) can be used while breastfeeding. The medication from the device won't hurt your baby, but you might notice a slight drop in your milk supply. Follow up with your provider about the best time to get the IUD inserted.
It's possible for your body to push the Mirena IUD (levonorgestrel) back out of your uterus into your vagina. If this happens, call your healthcare provider right away and use a back-up method of protection (e.g., condoms, diaphragms) until you have a new device placed.
The Mirena IUD (levonorgestrel) doesn't protect you from human immunodeficiency virus (HIV) or other sexually transmitted infections (STIs). Only abstinence and condoms can help protect you from STIs. Talk to your provider right away if this is a concern for you.
If you're thinking about becoming pregnant, talk with your provider about removing Mirena IUD (levonorgestrel). After the IUD is out, it's possible for you to become pregnant the next time you ovulate, which can take days or a few weeks.
More on Mirena IUD (levonorgestrel) tips

Frequently asked questions about Mirena IUD (levonorgestrel)

How to save using GoodRx




What are the risks and warnings for Mirena IUD (levonorgestrel)?
Mirena IUD (levonorgestrel) can cause some serious health issues. This risk may be even higher for certain groups. If this worries you, talk to your doctor or pharmacist about other options.

Ectopic pregnancy
Risk factors: Previous ectopic pregnancy | Past surgery performed on your fallopian tubes | Current pelvic infection
Ectopic pregnancies happen when a fertilized egg implants somewhere other than your uterus. They're very rare, but can be life-threatening and sometimes need to be treated with surgery. Progestin-only contraception, including the Mirena IUD (levonorgestrel) IUD, can raise your risk of ectopic pregnancies. Pregnancy is rare with all IUDs, but if you do become pregnant while the Mirena IUD (levonorgestrel) IUD is inserted, the chance of it being an ectopic pregnancy is high. If you experience unexplained or severe pelvic pain along with unusual vaginal bleeding, let your provider know.
If you do become pregnant after the Mirena IUD (levonorgestrel) IUD was placed, contact your provider right away. Your provider will recommend for you to remove Mirena IUD (levonorgestrel) because keeping it in place raises your risk for complications such as miscarriage and infection.

Sepsis (blood infection)
Risk factors: Placement of device in an unhygienic environment
Sepsis is when bacteria infect your bloodstream, and it can be life-threatening. Your risk of getting this infection goes up if Mirena IUD (levonorgestrel) wasn't placed using proper antibacterial technique. Sepsis would typically happen shortly after the device was inserted, sometimes even within a few hours. Tell your provider right away if you have pelvic pain, a high fever, or any other symptoms of being sick shortly after the device was placed.

Pelvic inflammatory disease (PID)
Risk factors: History of or current pelvic inflammatory disease | Current sexually transmitted infections | Multiple sex partners
IUDs raise your risk of developing pelvic inflammatory disease (PID) because there's always a small chance bacteria can get into your uterus when the device is placed. Because of this, the Mirena IUD (levonorgestrel) IUD isn't safe to use if you've ever had or are prone to PID. If you start to experience any unusual pelvic pain, funny-smelling discharge, unusual vaginal bleeding, sores or cuts in your genital area, or a high fever, call your provider right away.

Uterine injury
Risk factors: Placing the Mirena IUD (levonorgestrel) IUD less than 6 weeks after giving birth
There's a very small chance that the Mirena IUD (levonorgestrel) IUD can uterine injury (perforation), which is extremely dangerous. It also prevents the Mirena IUD (levonorgestrel) IUD from working properly, meaning you can get pregnant if this happens. The risk of perforation is higher if you've the Mirena IUD (levonorgestrel) IUD placed less than 6 weeks after you give birth to a baby. Your provider will need to remove the IUD if there's an injury, and this might require surgery. Tell your provider right away if you can't feel the threads that hang freely inside your vagina after it has been placed.

Body ejecting the device
Risk factors: Placing the Mirena IUD (levonorgestrel) IUD less than 6 weeks after giving birth
There is a small chance the body can eject the Mirena IUD (levonorgestrel) IUD from the uterus back into your vagina. If this happens, the device won't be working and you can get pregnant. Your risk of having this happen is higher if you have the IUD placed less than 6 weeks after you gave birth. If you notice your menstrual bleeding suddenly becomes heavier than usual, this could be a sign your body is ejecting the Mirena IUD (levonorgestrel) IUD. Tell your provider if this happens and use non-hormonal protection (e.g., condoms, diaphragms) until your provider places a new device or tells you the device is in the right place.

Irregular periods
The Mirena IUD (levonorgestrel) IUD can cause you to experience irregular menstrual periods. Most people will have heavier or longer periods for the first 3 to 6 months after the device is placed, followed by very light or no periods. But, you might notice changes of any kind to your menstrual cycle while using the Mirena IUD (levonorgestrel) IUD. If you're worried about the changes to your periods, talk to your provider, especially if you're having sudden or unusually heavy bleeding after the first 3 to 6 months. This could be a sign that the device is not in the correct place. If you don't get your period within 6 weeks of your last one, take a pregnancy test to make sure you aren't pregnant.

Ovarian cysts
Since Mirena IUD (levonorgestrel) is located within the uterus, it can sometimes lead to the development of ovarian cysts. Although most ovarian cysts don't cause any symptoms, some might cause pelvic pain or pain during sex. In most cases, the cysts go away on their own after a few months, but your provider will keep an eye on things just to make sure. Surgery is usually not required for these.

Possible risk of cancer
People who have or have had breast cancer shouldn't use hormonal birth control, including Mirena IUD (levonorgestrel). Certain types of breast cancer can be sensitive to hormones, and might grow in the presence of hormones.

Mirena IUD (levonorgestrel) dosage forms
Typical dosing for Mirena IUD (levonorgestrel)
Your provider will place Mirena IUD (levonorgestrel) inside the uterus at their office.
Prevent pregnancy: Mirena IUD (levonorgestrel) will stay in place for up to 8 years. Then, your provider will remove the IUD at their office.
Heavy menstrual bleeding: Mirena IUD (levonorgestrel) will stay in place for up to 5 years. Then, your provider will remove the IUD at their office.

Interactions between Mirena IUD (levonorgestrel) and other drugs
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amoxicillin
- Ampicillin
- Amprenavir
- Apalutamide
- Aprepitant
- Armodafinil
- Artemether
- Bacampicillin
- Betamethasone
- Bexarotene
- Bosentan
- Brigatinib
- Carbamazepine
- Carbenicillin
- Cefaclor
- Cefadroxil
- Cefdinir
- Cefditoren
- Cefixime
- Cefpodoxime
- Cefprozil
- Ceftazidime
- Ceftibuten
- Cefuroxime
- Cenobamate
- Ceritinib
- Clavulanic Acid
- Clobazam
- Cloxacillin
- Colesevelam
- Cyclacillin
- Cyclosporine
- Dabrafenib
- Darunavir
- Dexamethasone
- Dicloxacillin
- Doxycycline
- Efavirenz
- Elagolix
- Elvitegravir
- Encorafenib
- Enzalutamide
- Etravirine
- Fosamprenavir
- Fosaprepitant
- Fosphenytoin
- Griseofulvin
- Guar Gum
- Isotretinoin
- Ivosidenib
- Lesinurad
- Lixisenatide
- Lorlatinib
- Lumacaftor
- Minocycline
- Mitotane
- Modafinil
- Mycophenolate Mofetil
- Mycophenolic Acid
- Nafcillin
- Nelfinavir
- Nevirapine
- Octreotide
- Oxacillin
- Oxcarbazepine
- Oxytetracycline
- Penicillin G
- Penicillin G Procaine
- Penicillin V
- Phenobarbital
- Phenylbutazone
- Phenytoin
- Pitolisant
- Prednisone
- Primidone
- Red Clover
- Rifabutin
- Rifampin
- Rifapentine
- Ritonavir
- Rufinamide
- Secobarbital
- St John's Wort
- Sugammadex
- Sultamicillin
- Tazemetostat
- Telaprevir
- Tetracycline
- Theophylline
- Ticarcillin
- Tigecycline
- Tizanidine
- Topiramate
- Ulipristal
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acitretin
- Amitriptyline
- Atazanavir
- Clomipramine
- Diazepam
- Doxepin
- Eslicarbazepine Acetate
- Imipramine
- Lamotrigine
- Licorice
- Lorazepam
- Perampanel
- Prednisolone
- Selegiline
- Tacrine
- Temazepam
- Triazolam
- Troleandomycin
- Voriconazole
- Warfarin

Mirena IUD (levonorgestrel) contraindications
Pregnancy or suspicion of pregnancy
Use as emergency contraception
Certain abnormal uterine anatomy
Acute pelvic inflammatory disease (PID) or a history of PID
Postpartum endometritis or infected abortion in the past 3 months
Breast cancer or other progestin-sensitive cancer
Uterine bleeding without a known cause
Untreated inflammation of the cervix or vagina, or other lower genital tract infections
Liver disease or liver tumor
A previous intrauterine device (IUD) that hasn't been removed

What are alternatives to Mirena IUD (levonorgestrel)?
Prevent pregnancy for up to 8 years
Relieve heavy menstrual periods for up to 5 years

What is the latest news about Mirena IUD (levonorgestrel)?
Get savings updates for Mirena IUD (levonorgestrel)
Receive price alerts, news, and other messages from GoodRx about Mirena IUD (levonorgestrel) and other healthcare topics and relevant savings offers.By providing your email, you consent to receive marketing communications from GoodRx, which may include content and/or data related to men’s health, women's health, reproductive care, or sexual health. You agree to the GoodRx Terms of Use and acknowledge the Privacy Policy. You can unsubscribe at any time.
References
Best studies we foundAmerican College of Obstetricians and Gynecologists. (2023). Postpartum birth control.
Bayer. (2023). IUDs and other birth control options.
Bayer HealthCare Pharmaceuticals Inc. (2022). Mirena- levonorgestrel intrauterine device [package insert]. DailyMed.
Centers for Disease Control and Prevention. (2023). Contraception.
Browse medications
View AllResearch prescriptions and over-the-counter medications from A to Z, compare drug prices, and start saving.