Key takeaways:
Knee replacements can help with pain, stiffness, and limited mobility due to different types of arthritis.
Other treatments — such as medication, physical therapy, and more — are often recommended before you can get a knee replacement.
A knee replacement is a big surgery and it’s not right for everyone. Your surgeon and primary care provider can help you decide if it’s the right treatment for you.
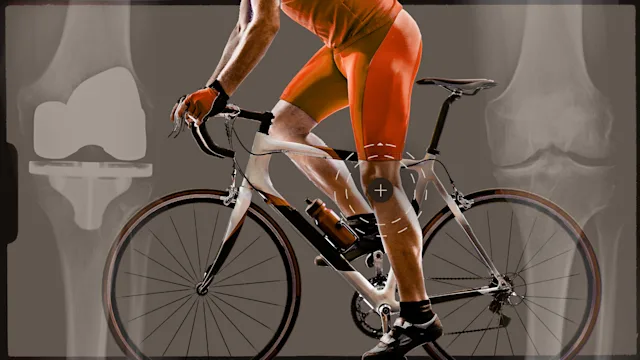
If you’ve struggled with knee pain — especially for a long time — you might be wondering what to do about it. Knee pain can affect your daily activities and limit the things you love to do. So, it makes sense to want to get rid of it for good.
Knee replacement surgery, also known as knee arthroplasty, is a good way to do that. It helps relieve symptoms due to different types of arthritis, most commonly osteoarthritis — but it’s not right for everyone. It’s usually reserved for where all other treatment options have failed.
So how do you know if a knee replacement is right for you? Let’s dive in.
Symptoms
If you’re reading this, you (or a loved one) probably have the most common symptom of knee arthritis: pain.
Other symptoms can include:
Pain that worsens with activity
Stiffness, especially after rest
Swelling
Limited motion
Clicking, crunching, or grinding sensations or sounds
Changes in the way your knee looks (sometimes)
Quiz: Do I need knee replacement surgery?
How do you diagnose arthritis?
There are many reasons to have knee pain. It may be osteoarthritis, but that’s not the only cause.
The knee isn’t a complicated joint, but there are a lot of structures in and around it that can cause pain. For example, ligaments, tendons, or menisci (cartilage between the bones) could be the cause of your symptoms. So, the first step is to determine the cause of your knee pain. If you’ve never seen a medical professional about it, now’s the time.
“Arthritis” means there’s inflammation in your knee joint. But it’s important to dig a little deeper. What type of arthritis is it? Is the inflammation caused by an underlying disease (inflammatory arthritis), or is it caused by breakdown of cartilage in your joint (osteoarthritis)? Understanding the difference will be important in determining the best treatment plan.
Recovery after knee replacement surgery is hard work. Three people describe what to expect after getting a new knee.
Being prepared before surgery can make a big difference. These eight tips can help make your recovery go smoothly after knee replacement.
Not ready for a knee replacement despite your knee pain? Learn about the types of injections that might help relieve your pain.
A clinical expert, like your primary care provider or an orthopedic specialist, can help you find the likely cause of your knee pain. They’ll ask questions about your pain, activity history, and any past knee injuries. They’ll also examine your knees. These steps, combined with X-rays, are usually enough to diagnose osteoarthritis.
If the diagnosis is unclear, more testing can help. Sometimes additional imaging, such as an MRI or ultrasound, is useful. A clinician might also drain fluid from your knee to test it. This can help rule out an infection or gout.
Your primary care provider might refer you to a rheumatologist if they suspect an inflammatory cause of your knee pain. This might include rheumatoid arthritis or psoriatic arthritis.
Read more like this
Explore these related articles, suggested for readers like you.
Treatments
Knee replacement surgery is a big surgery — especially if you have other medical problems. And it requires a few months of rehab afterwards. Because of this, it’s best to try conservative treatments first. While it’s common to brush these options off, there’s a lot of research to show that they help.
Specific treatment plans vary depending on the cause of your pain and the severity of your symptoms. But conservative treatment options include the following.
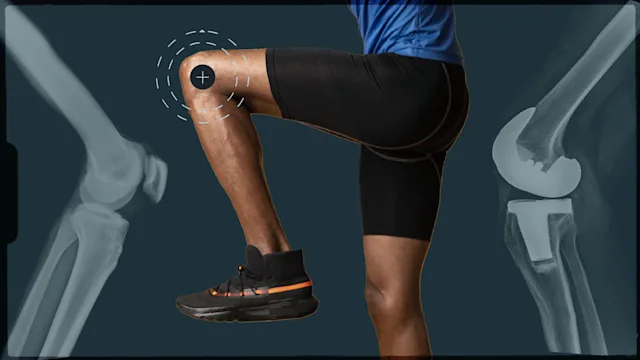
Physical therapy and exercise
Physical therapy (PT) and exercise are essential for managing knee pain due to arthritis. Here’s why exercise and PT are important.
When something’s “off” in the knee joint, it’s common for muscles around your knee to shut down and weaken. The weaker your muscles are, the more pain, instability, and difficulty you’ll have when trying to use that joint. It’s a classic “use it or lose it” scenario.
Whether or not you end up having a knee replacement, exercises are key to maintaining movement, function, and even balance.
Medications
Both prescription and over-the-counter medications can help with inflammation and pain. Here are some options to consider:
Oral nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or meloxicam
Topical anti-inflammatory creams
Acetaminophen (Tylenol), which is an option for those who can’t take NSAIDs
The best option for you depends on any other medical problems you have, and/or the medications you already take.
Topical and oral NSAIDs are more effective than acetaminophen for osteoarthritis pain. But they come with a higher risk of side effects.
Beyond these options, there are now powerful medications available to treat inflammatory types of arthritis like rheumatoid arthritis and improve peoples’ day-to-day function. These medications are called DMARDs (disease-modifying antirheumatic drugs) and include:
Traditional, or conventional DMARDs, including pills like methotrexate, hydroxychloroquine, leflunomide, and sulfasalazine
Biologic DMARDs, like Humira, Enbrel, and Cimzia, which are medications you get as an injection or infusion
Janus kinase (JAK) inhibitors, like tofacitinib (Xeljanz), upadacitinib (Rinvoq), baricitinib (Olumiant), and more, which are newer medications that you take as a pill
Knee injections
An injection into your knee joint is also an option for many. An experienced medical professional can do an injection to deliver medication right to the source of your pain.
The injection usually includes a steroid (a powerful anti-inflammatory) and a numbing medication.
Other options, like hyaluronic acid, are a bit more controversial, so recommendations vary by person.
Weight loss
If excess weight is contributing to your knee problems, weight loss can ease your symptoms, especially in combination with the other treatments listed above. That said, weight loss is hard and looks different for everyone. So, don’t be afraid to ask for help.
When is it time?
There’s a reason approximately 700,000 knee replacement surgeries are performed every year in the U.S. Sometimes, medications and exercise aren’t enough. If you’re still having pain despite trying other treatments, it might be time to consider surgery. Everyone’s tolerance for pain is different, and everyone’s functional needs are different. Only you know what your symptoms and limitations are.
What questions should you ask your doctor about knee replacement?
Try to get as much information as you can before deciding on surgery. One way of doing this is by speaking with others who’ve had a knee replacement to find out more about their experience.
Working with a trusted physical therapist before making a decision can also be helpful. They’ll have more insight on what you might be able to expect in your recovery.
You can also ask your surgeon questions such as:
What’s your experience with knee replacements?
What are the risks of surgery?
What will my pain be like after surgery?
How long will rehab take?
What type of help should I have at home?
Frequently asked questions
Both conditions affect your joints, but there are many differences between the two. Rheumatoid arthritis can cause inflammation throughout your entire body, including all joints.
Osteoarthritis, on the other hand, commonly affects larger joints (like your hip and knee) and it doesn’t go beyond the joints.
Orthopedic surgeons perform knee replacement surgeries. But it’s best to get a diagnosis first:
Your primary care provider can help with that and/or suggest an orthopedic referral.
If you already know you have osteoarthritis, you can see an orthopedic surgeon.
If you have inflammatory arthritis (like rheumatoid arthritis), speak with your rheumatologist about surgery first. They can guide you to available surgeons.
The two types of knee replacement are complete and partial. There are three compartments in your knee, and the location of the damage will determine whether you need the whole joint replaced or just part of it.
There are also different types of materials used in the implants. Your surgeon can provide more details on this, as it depends on their experience, your activity level and age, and the track record of the implant.
Both conditions affect your joints, but there are many differences between the two. Rheumatoid arthritis can cause inflammation throughout your entire body, including all joints.
Osteoarthritis, on the other hand, commonly affects larger joints (like your hip and knee) and it doesn’t go beyond the joints.
Orthopedic surgeons perform knee replacement surgeries. But it’s best to get a diagnosis first:
Your primary care provider can help with that and/or suggest an orthopedic referral.
If you already know you have osteoarthritis, you can see an orthopedic surgeon.
If you have inflammatory arthritis (like rheumatoid arthritis), speak with your rheumatologist about surgery first. They can guide you to available surgeons.
The two types of knee replacement are complete and partial. There are three compartments in your knee, and the location of the damage will determine whether you need the whole joint replaced or just part of it.
There are also different types of materials used in the implants. Your surgeon can provide more details on this, as it depends on their experience, your activity level and age, and the track record of the implant.
The bottom line
Knee replacement surgery is very effective in relieving knee pain, stiffness, and mobility problems due to arthritis. If you have a diagnosis of arthritis, it’s best to try nonsurgical treatments first. Medication, strengthening exercises, and assistive devices can make a big difference to your symptoms. But if other treatments don’t work well enough or stop working, a knee replacement might be an option for you. A primary care physician or orthopedic specialist can help you determine your next best steps.

Why trust our experts?


References
Altman, R. D., et al. (2022). Missing the mark? American College of Rheumatology 2019 guidelines for intraarticular hyaluronic acid injection and osteoarthritis knee pain. The Journal of Rheumatology.
American College of Rheumatology. (n.d.). Rheumatologist.
Kahlenberg, C. A. (2024). Knee replacement. Hospital for Special Surgery.
Katz, J. N., et al. (2021). Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA.
Rice, D. A., et al. (2011). Mechanisms of quadriceps muscle weakness in knee joint osteoarthritis: The effects of prolonged vibration on torque and muscle activation in osteoarthritic and healthy control subjects. Arthritis Research & Therapy.
Robson, E. K., et al. (2020). Effectiveness of weight-loss interventions for reducing pain and disability in people with common musculoskeletal disorders: A systematic review with meta-analysis. Journal of Orthopaedic & Sports Physical Therapy.
Sheth, N. P., et al. (2024). Total knee replacement. OrthoInfo.
Throckmorton, T. W. (2022). What is an orthopaedic surgeon? OrthoInfo.
Worcestershire Knee and Hip Clinic. (n.d.). Anatomy of the knee.
Yale Medicine. (n.d.). Musculoskeletal ultrasound.
Zeng, C., et al. (2021). Comparative efficacy and safety of acetaminophen, topical and oral non-steroidal anti-inflammatory drugs for knee osteoarthritis: Evidence from a network meta-analysis of randomized controlled trials and real-world data. Osteoarthritis and Cartilage.