Key takeaways:
Stress can impact the gastrointestinal system in many different ways. This includes changing the way the stomach and intestines digest, which can lead to heartburn symptoms.
Taking small steps to reduce your stress levels can have a big impact on both your mental and physical health. But if you are experiencing frequent heartburn, there are several tips and treatments that can help alleviate your symptoms, too.
It is important not to ignore heartburn. It could be related to underlying gastroesophageal reflux disease (GERD) or peptic ulcer disease (PUD), conditions that can have long-term health risks when left untreated.
Have you ever felt that a stressful situation was giving you heartburn? Or heard someone say their boss was giving them an ulcer? Many people have experienced the different ways that mental health can impact digestion, but is it possible for stress to actually cause heartburn? The answer is yes, definitely!
Before we dive into the relationship between stress and the digestive tract, let’s talk about the term “heartburn.” When people use this term, they are usually referring to the symptoms of acid reflux, or gastroesophageal reflux disease (GERD). GERD can cause many different symptoms, and one of them is a burning feeling in the chest, resulting from acid from the stomach traveling up into the esophagus.
Peptic ulcer disease (PUD) is a little different; it involves erosions in the lining of the stomach or intestine. When this happens, it tends to cause pain in the stomach area or upper abdomen, rather than a burning in the chest. But there is a lot of overlap in these two conditions, and people may experience both as heartburn. Here, we’ll review how stress can lead to both conditions.
How does stress affect the body?
To understand how stress causes heartburn, it helps to first understand a few things about the nervous system. There is a part of the nervous system — called the autonomic nervous system — that controls many different processes inside the body. This includes everything from heart rate to digestion.
The autonomic nervous system is further divided into two parts:
The sympathetic system: This controls how the body responds to stress or a threat, which is often referred to as the “fight or flight” response.
The parasympathetic system: This controls processes that happen when the body is relaxed, or in a kind of recovery mode. It does things like lower our heart rate and blood pressure, and allows us to urinate and pass a bowel movement.
When someone is under stress, the body interprets it as a threat to survival. Even if we are not truly fearing for our lives, the reaction is the same — even if the stress is just coming from a busy work day or traffic jam. When this happens, the sympathetic nervous system goes to work. It tells the body to put digestion on hold, so that energy can be diverted to things like pumping the heart and fueling the muscles. Stress has an immediate effect on the way your stomach works.
How are stress and heartburn linked?
Studies show that stress affects the stomach in the following ways:
The muscle in the walls of the stomach becomes less active.
Less stomach acid is produced.
Glands that help to protect stomach lining are less active.
While the digestive system is designed to handle temporary disruptions in these processes, chronic stress can result in more significant digestive problems. People may have increased burping and stomach upset when their food is not properly digested. The protective lining of the stomach can also become thinner and inflamed. And ongoing damage to the stomach lining by acid can eventually cause an erosion, or ulcer, of the stomach.
But these are not the only ways that stress can contribute to heartburn. People can develop behaviors that aggravate symptoms of heartburn, such as:
Eating patterns and meal times may become more erratic.
Some people find that they have a reduced appetite, while others find that they tend to eat more when under stress.
Some people gravitate to less healthy food options, such as fast foods.
Someone’s alcohol intake may increase, which can inflame the stomach lining and lead to gastritis.
Many people engage less in healthy activities such as exercise. Being upright and active greatly assists digestion through the effects of gravity and muscle activity.
What can I do about stress?
Stress causes real, physical reactions in the body. So when we take action to reduce stress, it produces real, physical benefits. When returning to a more relaxed state, the parasympathetic nervous system goes into action. This allows the body to restore the protective lining of the stomach and improve digestion.
There are also some basic habits that can help to reduce stress, which include:
Regular exercise
Spending time in nature
Decreasing use of social media
Activities that promote peaceful feelings, such as meditation
Counseling and therapy, alone or in combination with medication, can also be very helpful for improving stress and mental health. There are a number of potential medications, particularly ones for depression, that can help people with their mood and anxiety levels.
How can I relieve heartburn?
If you are experiencing heartburn, there are some daily changes you can make to help improve your symptoms:
Try to limit foods and drinks that can aggravate your symptoms. This usually includes highly acidic foods, like citrus fruits and tomatoes. Vinegar and vinegar-based foods, like pickled foods, marinades, and sauces, can also be aggravating.
Limit or avoid alcohol intake. Even if you don’t feel ready to abstain completely, cutting back may make a big difference.
Avoid going to bed with a full stomach. A good rule of thumb is to eat at least 2 hours prior to lying down to sleep.
When these measures aren’t enough, there are also medications which can help to reduce heartburn:
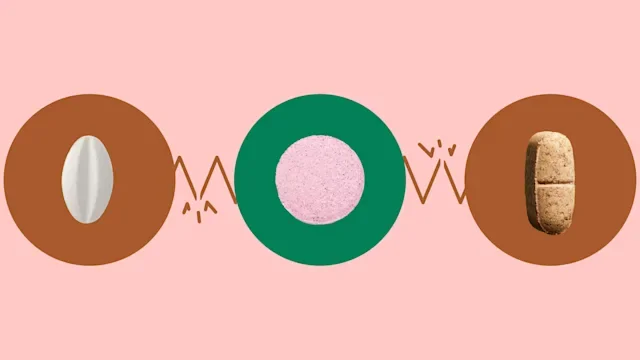
Antacids: These usually contain calcium carbonate or magnesium. They come in multiple different forms, including tablets, chewables, and liquids. They work to quickly neutralize stomach acid, but do not actually prevent acid reflux.
H2 blockers: These medications work by blocking histamine, one of the body chemicals that stimulate the stomach to make acid. H2 blockers can be taken to provide relief with an acid reflux attack, and can be taken for short periods to reduce stomach acid.
Proton pump inhibitors: These are the most definitive treatments for heartburn relief and are available in over-the-counter and prescription-strength versions. They work by blocking an enzyme involved in the production of stomach acid and are the best option for preventing acid reflux and healing stomach ulcers.
If you find you need these medications consistently for more than 2 weeks, it is a good idea to talk to your medical provider. They can run some tests to look for other conditions that may be contributing to your symptoms.
Can stress and heartburn affect my long-term health?
Stress has wide-reaching effects on both your mental and physical health. The connection between stress and acid reflux can also have several health consequences that arise from the long-term effects of acid on the stomach and esophagus. These include:
Gastrointestinal bleeding from ulcers, which can be life-threatening in severe cases
Barrett’s esophagus, which can develop into esophageal cancer
While these problems may sound scary, they can usually be avoided with treatment and self-care. It is very important to recognize when stress is affecting how you are feeling mentally and physically. Often it is necessary to seek help to feel your best.
The bottom line
We all experience stress in our lives. In fact, it’s important to feel stress sometimes. Stress warns our body of situations that may be unsafe. But when stress is an ongoing issue, it can take a toll on our health. And the digestive system commonly absorbs the impact. If you are feeling stressed and experiencing heartburn symptoms, there are lifestyle changes you can make right away that can help. These healthier habits can have multiple positive effects on the body.
If your symptoms are not getting under control quickly, it is important to make an appointment to see your medical provider. There you can discuss your symptoms and hear about treatment options tailored to you.

Why trust our experts?


References
Browning, K. N., et al. (2014). Central nervous system control of gastrointestinal motility and secretion and modulation of gastrointestinal functions. Comprehensive Physiology.
Labanski, A., et al. (2020). Stress and the brain-gut axis in functional and chronic-inflammatory gastrointestinal diseases: A transdisciplinary challenge. Psychoneuroendocrinology.