Key takeaways:
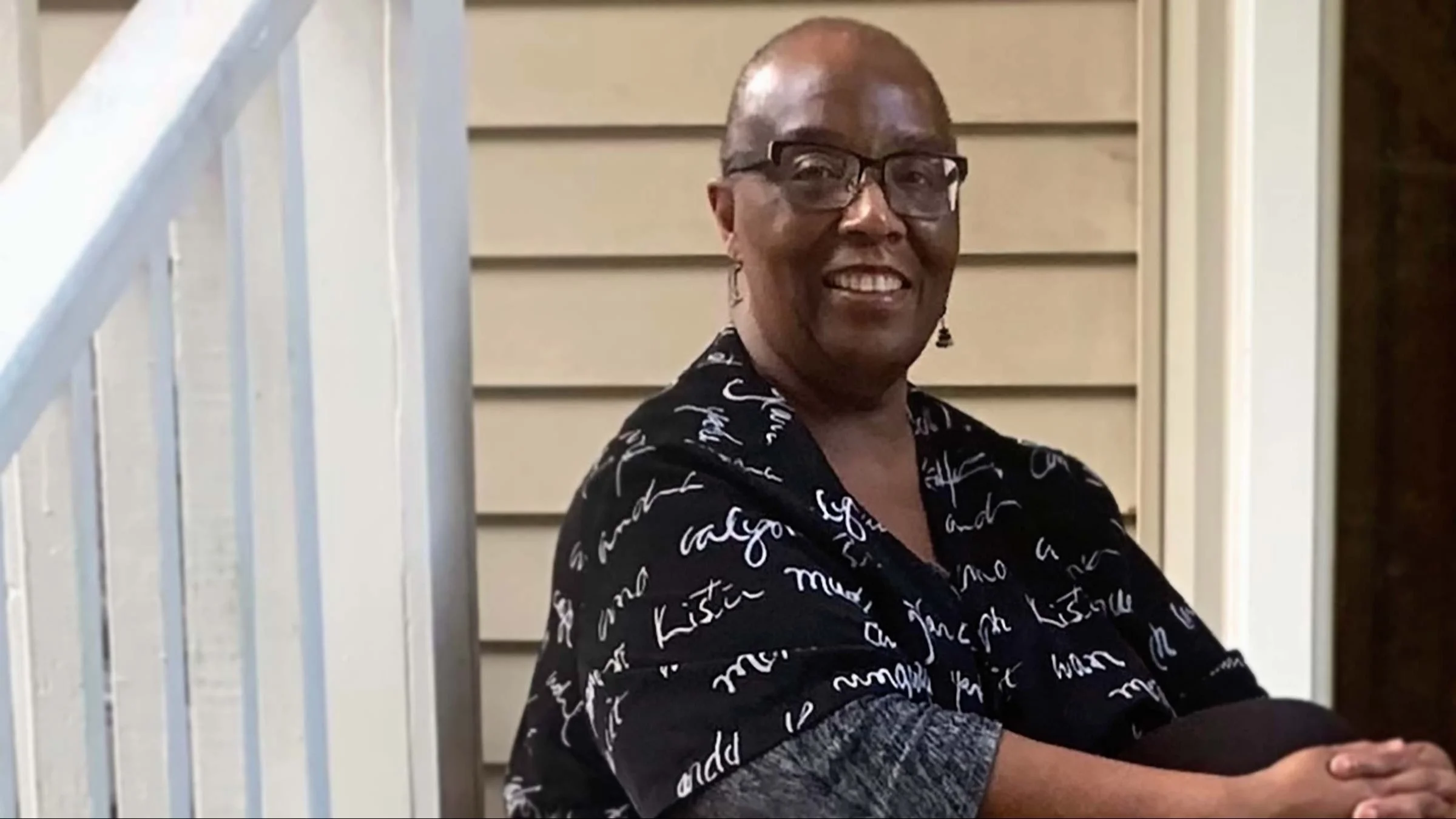
When Angela Jones had a tummy tuck, she thought it would take her a month to recover.
But complications, including a buildup of fluid in her soft body tissues, slowed her down for nearly a year.
Today, she has learned to manage her chronic lymphedema and lipedema conditions by taking a holistic approach.
Angela Jones first noticed the swelling about 4 months after her abdominoplasty (also known as a tummy tuck) in August 2019.
“I noticed that I had this, like, pocket of swelling on my inner right thigh,” she says.
She also noticed the swelling was increasing. Whereas once she’d walk 5 miles a day, she now could barely make it down the driveway and back at her Raleigh, North Carolina, home. Her physical therapist suspected lymphedema, which is an abnormal swelling of soft body tissues that most commonly occurs in arms and legs. It develops when the flow of the colorless, watery fluid called lymph is blocked or impaired.
“Everything was going well [with the abdominoplasty], but then I became septic (infected) about a week and a half after surgery,” she says. “And so, I was in the hospital for that. Then they found that I was just very, very anemic.”
That meant she had a potentially life-threatening infection, and the anemia left her weak and tired. After a blood transfusion, her care team discharged her from the hospital, but full recovery from her surgery was slow because of abdominal swelling, she says.
“You would think with swelling, if you eliminate the things that cause the swelling, you could get rid of the swelling,” says Angela, a former registered nurse. “But that’s not how it works with lymphedema, because it’s a different kind of swelling.”
A rough recovery after a tummy tuck
When she had her tummy tuck, her surgeon removed about 12 pounds of excess fat from her stomach area. Angela, who is completing wellness and holistic nutrition courses in Arizona, figured her surgery and recovery would take about 30 days. However, her month-long trip home to Raleigh turned into 11 months of recuperation.
Contributing to the lymph buildup in her body was post-surgical wound care. Her surgical scars were slow to heal, she says, and her prescribed wound care treatment included hours of lying relatively motionless in a recliner, for weeks at a time. Concerned about the swelling, her provider wanted to first rule out edema (swelling of the body tissues) and prescribed a diuretic, or a water pill.
After 2 weeks of no decrease in swelling and discomfort, Angela’s physical therapist, who’d seen the condition in other clients, suggested she had lymphedema.
- PrednisoneGeneric Deltasone and Rayos and Sterapred
- MicrozideHydrochlorothiazide
- MedrolMethylprednisolone
Specialist diagnoses both lymphedema and lipedema
Angela went to a lymphedema specialist in neighboring Durham, who diagnosed both lymphedema and lipedema — an associated disorder that doesn’t involve the lymphatic system but involves fatty deposits in legs and sometimes arms. The specialist estimated that Angela had developed lipedema sometime in her 30s.
“I used to lose weight and wonder why my thighs wouldn’t go down,” she says, “but when I had [my tummy tuck] done in 2019, it triggered it and actually exacerbated it because I also got an infection that I had to fight. So right now, I’m trying to get both conditions to coexist — peacefully.”
Trying a holistic approach to healing
One way of focusing on her wellness is spending much of the year in Tempe, Arizona. North Carolina is hot and humid from late spring through early fall, conditions that can cause blood vessels to dilate (expand) and move more fluid to lymphedema-affected limbs.
Angela initially took up temporary residence in Tempe to study holistic nutrition, wellness, and life coaching. She’s since enrolled in an additional program called Mind Body Wellness, because she likes the holistic approach to healthcare.
“I like that holistic looks at the entire body, not just the presenting symptoms,” she says.

To keep the swelling under control, Angela uses both mechanical and manual means every day. For mechanical relief, Angela uses a therapeutic compression pump garment that gently squeezes and releases affected areas to stimulate lymph fluid movement and drainage. She also uses a massage gun and a vibration platform, also called a vibration plate, which assists blood flow.
Manual means include walking about a quarter of a mile each day. Before the tummy tuck, she’d walk 4 or 5 miles a day. But exercise increases inflammation, so she does what she can.
She also does dry skin brushing 5 to 10 minutes every morning, which involves massaging the skin on her legs, arms, stomach, and chest with a dry, stiff-bristled bath or shower brush. Wellness practitioners promote the technique as a means to unclog pores and exfoliate skin right before a shower. Dry skin brushing also stimulates the lymphatic system by increasing blood circulation and lymph drainage.
She’s changed some of her eating habits, too. “I drink a lot of water, and I don’t eat sugar anymore,” she says. “If I eat anything sweet, it’s a very limited amount.” She also avoids foods she finds irritate her conditions, such as certain apple varieties, dairy products, and highly processed, simple carbs like white bread and pasta.
Learning to manage her chronic conditions
Both lymphedema and lipedema are chronic, incurable conditions. Angela has learned of surgeries that might improve symptoms, but she’s not interested.
“I figure with the things I’m doing, I’m managing both conditions really well,” she says. “So, I’m not interested in having surgery, because both surgeries are kind of high risk, and I’ve had my share. So, I don’t want to do that.”
Angela also shares her experiences and educates others as part of a monthly lymphedema panel that meets via Zoom. People log in and ask questions about how she and others manage to live with the condition. “One thing I always say is, what works for me may not necessarily work for you.”
“I don’t look at it anymore as a bad thing. Of course, I don’t look at it as a good thing, either,” she laughs. “I look at the fact that — you know what? It could be worse, because there are some people who have either condition or both conditions and they’re not even mobile. They have to have help with everything. So, what keeps me on track is the fact that it could be so much worse, and I feel like I’m blessed to have it where it is.”
“It just comes down to listening to your body. Listen to your condition. What is it telling you to do to manage it? I think that somewhere in that problem lies the solution.”

Why trust our experts?