Key takeaways:
New research from GoodRx Research and collaborators from Harvard Medical School finds that areas that lack adequate access to healthcare are also more likely to lack access to internet services.
Counties with relatively low access to healthcare and internet are more likely to be rural and have lower median household income, compared to counties with better access.
Without improved internet access, efforts to expand telemedicine may have limited effectiveness, especially in counties where these services are most critically needed.
Telemedicine has been touted as a potential solution to healthcare deserts — places where residents don’t have adequate access to traditional healthcare infrastructure like pharmacies, primary care providers, hospitals, and community health centers.
But what happens if healthcare deserts are also internet deserts? While telemedicine allows healthcare providers to see patients who live much farther away, those patients still need a stable internet connection.
New data from the GoodRx Research Team, in collaboration with researchers from Harvard Medical School and published in the Journal of the American Medical Association (JAMA) Network Open, shows that areas with more healthcare deserts are more likely to be internet deserts as well.
Areas with poor access to both healthcare infrastructure and internet services are also more likely to be rural and have lower household incomes.
Rural, lower-income areas are more likely to lack both healthcare access and internet access
To analyze the presence of internet deserts and healthcare deserts in a given region, we calculated the population-weighted average number of healthcare deserts and compared that to the share of the population without any internet subscription (broadband, cellular, satellite, etc.).
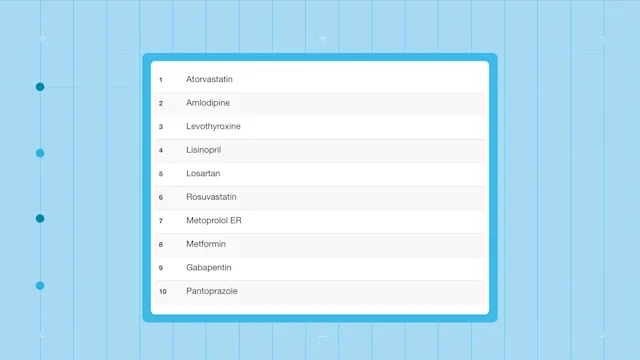
To identify healthcare deserts, we evaluated areas based on whether they had six different types of healthcare infrastructure: pharmacies, primary care providers, hospitals, hospital beds, trauma centers, and health centers.
Grouping metropolitan (50,000 people or more), micropolitan (10,000 to 50,000 people), and non-metropolitan or micropolitan (less than 10,000 people) areas in each state together, we identified a positive relationship between the prevalence of people without internet access and the expected number of healthcare deserts in a region. In other words, places with more healthcare deserts also had more people without internet access. In particular, rural regions had higher rates of internet deserts as well as higher numbers of healthcare deserts, compared to urbanized areas.
For example, people who live in rural Arizona, New Mexico, and South Carolina can expect to face at least three different types of healthcare deserts on average, while over 37% of the population in these areas doesn’t have any kind of internet subscription. Meanwhile, those living in metropolitan areas can expect fewer than two types of healthcare deserts on average, and less than 25% of the population lives without internet access.
We also examined differences in county-level characteristics across places with and without healthcare access and internet access. As detailed in the table below, we found that counties with above-median numbers of healthcare deserts and lack of internet access were more likely to be rural (78% versus 26%) and have lower median household income ($47,333 versus $66,139).
The strongest correlation between expected number of healthcare deserts and county-level characteristics was the rural population percentage. Echoing the figure above, rural areas appear to be the most impacted by both healthcare and internet deserts.
Summing it all up
While telemedicine has the potential to improve health disparities by bringing care to those who lack access to traditional healthcare infrastructure, it could also exacerbate disparities in regions without universal internet access. To avoid widening the divide in healthcare access between urban and rural areas, telemedicine expansion must be accompanied by improvements to internet access and digital literacy.
Read about our study methods and all of our findings in the full research letter published in JAMA Network Open here.
Co-contributor: Jeroen van Meijgaard, PhD

Why trust our experts?