Key takeaways:
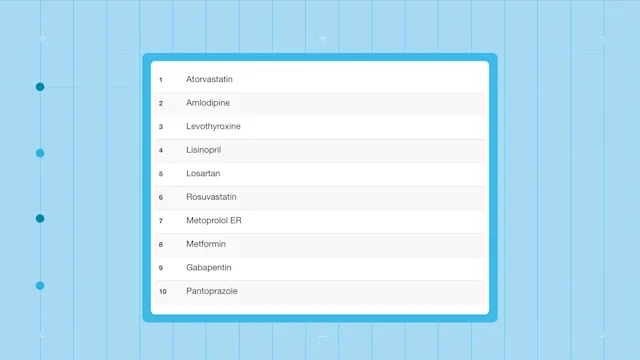
A GoodRx analysis looked at fills for medications that have been shown to possibly make COVID-19 symptoms worse (ACE inhibitors and ARBs) or potentially treat the virus (hydroxychloroquine, chloroquine, and azithromycin).
Fills for lisinopril (an ACE inhibitor) and losartan (an ARB), popular drugs that treat high blood pressure and heart failure, have fallen below normal levels, but not as much as other commonly prescribed medications.
Fills for hydroxychloroquine and chloroquine surged in the first weeks of March and have stayed at elevated levels since.
As we gain more knowledge on what medications have benefits or risks for COVID-19, patients should always talk with their doctors before making any changes to their medication regimen.
Introduction
When it comes to COVID-19 treatments, there has been little consensus among researchers, politicians, and the media on what is most effective. In the early days, hydroxychloroquine, chloroquine, and azithromycin were touted as three of the most promising new treatments, yet recent research reveals new safety concerns. Conversely, early on in the pandemic, angiotensin-converting-enzyme inhibitors (ACE inhibitors) and angiotensin II receptor blockers (ARBs), classes of drugs that treat high blood pressure and heart failure, were reported to potentially exacerbate COVID-19 symptoms.
Doctors and researchers have feared that this information could lead to an uptick in prescription fills for hydroxychloroquine and chloroquine and a drop in fills for ACE inhibitors and ARBs. New data from the GoodRx Research Team in collaboration with researchers from Harvard University and published in The Journal of the American Medical Association (JAMA), shows that fills of hydroxychloroquine spiked 210% in mid-March amid discussion about research related to their ability to treat COVID-19. However, despite concerns about their impact on COVID-19, fills for ARBs and ACE inhibitors have remained higher than expected and have tracked prescriptions for other medications filled for chronic conditions.
Fills for ACE inhibitors and ARBs
ACE inhibitors and ARBs are important medications to control blood pressure, treat people with heart failure and diabetic nephropathy, and prevent stroke. Healthcare practitioners have been concerned that people who need these medications most may have stopped taking them due to potential COVID-19 related risks. Forgoing medications (also known as non-adherence) can inadvertently increase health risks for patients with high blood pressure.
Luckily, fears of these possible risks did not seem to affect fills for ACE inhibitors and ARBs. Like all drugs, these high blood pressure medications spiked early on in the pandemic as people stocked up on their medications. Fills subsequently declined, but these declines were smaller than for other medications. In recent weeks, fills for these ARBs and ACE inhibitors have stabilized at or slightly below levels seen last year during the same period, suggesting that patients are continuing to take these medications.
Fills for hydroxychloroquine, chloroquine, and azithromycin
Prescription fills for hydroxychloroquine and chloroquine surged in the first weeks of March and have stayed at elevated levels since. The antibiotic azithromycin also experienced a small increase in prescription fills, especially compared to another common antibiotic, amoxicillin. But fills for azithromycin have declined substantially in recent weeks.
The stockpiling and use of unproven treatments like hydroxychloroquine and chloroquine can have unintended negative consequences for patients. In addition to the potentially harmful and even fatal health side effects, stockpiling these drugs has caused shortages, making it difficult for patients with lupus and rheumatoid arthritis to access the medication they need.
Summing it all up
While we saw a spike in fills for the much-publicized, unproven COVID-19 treatments hydroxychloroquine and chloroquine, we have not seen a large drop in prescription fills for essential heart medications, despite early concerns about possible COVID-19-related risks.
Though the continued level of fills for ARBs and ACE inhibitors is a good sign, it is possible that some decided not to take the medication after filling. Adding or stopping a medication without consulting a healthcare professional can be dangerous and potentially fatal. Patients should always have a discussion with their doctor before making any changes to their medication regimen. Although the pandemic has impacted access to in-person doctor visits, patients can still get advice from healthcare professionals through telemedicine.
Read the full research letter published in JAMA here.
Read more like this
Explore these related articles, suggested for readers like you.
Co-contributors: Diane Li, Amanda Nguyen PhD
Methodology
Using a sample of U.S. prescription fills, we compared weekly fills for each drug from February 16 through April 25, 2020 to average weekly fills during the same period in 2019. We compared fills for 10 of the most commonly prescribed drugs, hydroxychloroquine/chloroquine combined, and azithromycin.

Why trust our experts?