Key takeaways:
Ascites is a buildup of fluid in the abdomen (belly). It’s a complication of other serious medical conditions like cirrhosis, heart failure, or cancer.
Symptoms of ascites include weight gain, shortness of breath, and feeling full. This is due to the excess fluid in the belly.
The treatment for ascites includes draining the fluid, limiting sodium intake, and taking diuretics.
Ascites is an abnormal buildup of fluid in the abdomen (belly). Normally, you have just enough fluid in the abdomen to allow your organs to slide over each other when breathing and moving. When too much fluid builds up, it can be a sign of a serious illness.
What causes ascites?
Ascites is almost always a symptom of a serious health condition. It develops when pressure in the blood vessels of the liver gets too high (portal hypertension). It can also occur when levels of albumin (protein in the blood) get too low. Here are some common reasons for ascites.
Cirrhosis
Cirrhosis is the permanent scarring of liver tissue. It causes about 80% of ascites cases in the U.S. The scarring makes the liver hard, so the blood vessels can’t expand normally. Blood can’t easily pass through these blood vessels, so it backs up and pressures rise. The vessels then become leaky and fluid seeps out into the abdomen.
Search and compare options
Common causes of cirrhosis include:
Alcohol overuse
Heart failure
Heart failure means that the heart can’t pump blood the way it normally does. Blood gets backed up in the blood vessels of the lungs, liver, and other tissues. The buildup causes increased pressure in the vessels, and they begin to leak in the tissues and the abdomen.
There are many causes of heart failure, like:
Heart attacks
High blood pressure
Lung disease
Blood clots
Heart valve problems
Cancer
Cancer can also lead to ascites. There are two main ways cancer can cause ascites. Cancer can spread to the lining of the organs, causing them to leak fluid into the abdomen. Or a cancer can spread directly to the liver and cause scarring.
Read more like this
Explore these related articles, suggested for readers like you.
The most likely cancers to cause ascites are:
Ovarian
Liver
Pancreatic
Colon
Cancer treatments can also cause ascites. Chemotherapy and radiation therapy can cause inflammation in the liver and lead to scarring.
Other causes
There are other less common causes of ascites. These can include:
Kidney failure
Pancreatitis
Tuberculosis
Congenital liver disease
Malnutrition
What are the risk factors for ascites?
The risk factors for developing ascites are often the same ones that put you at risk for cirrhosis. Some of the most common risk factors include:
Alcohol overuse: increases the risk of cirrhosis
IV (intravenous) drug use: increases the risk of hepatitis and cirrhosis
Unprotected sex: increases the risk of hepatitis and cirrhosis
Nonalcoholic fatty liver disease: increases the risk of cirrhosis
What are the earliest symptoms of ascites?
The symptoms of ascites are often in line with how much fluid is in the belly. Some of the earliest symptoms of ascites that you might notice include:
Increase in waistline or abdominal girth: As fluid builds up, the waistline gets larger. The belly might be soft early on, but as more fluid leaks, it may feel hard to the touch.
Weight gain: As the fluid builds up, you might notice you’ve put on some pounds.
Feelings of fullness: The fluid can press on the stomach, making you feel full. This can make it harder for you to eat a whole meal.
Shortness of breath: Fluid that is building up in the abdomen might also be leaking in the lungs. It can also press on your lungs, making them harder to expand.
Many people with cirrhosis, heart failure, or cancer know they have a medical condition before they develop ascites. But for some people, ascites might be the first sign that something is wrong.
How do you diagnose ascites?
Your healthcare provider may be able to diagnose ascites in their office with a physical exam. They can check your belly for swelling by pushing on it and listening for a dull sound when tapping on it.
After diagnosing ascites, your provider will want to find out the cause. Some tests they may use include:
Ultrasound: An ultrasound can help see how much fluid is in the abdomen.
CT or MRI: CT and MRI not only show how much fluid has built up, but they can also show if there’s an abnormal mass (suggesting cancer).
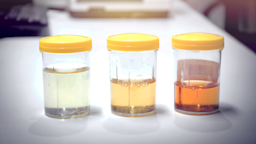
Paracentesis: A provider places a small needle through the abdominal wall to drain the fluid. Then they send it to the lab to look for protein, blood, bacteria, or cancer cells.
Lab tests: Blood tests can include complete blood counts and tests for hepatitis, liver, and kidney function.
How do you treat ascites?
Treatment for ascites depends on the underlying cause. In most cases, your healthcare provider will begin with:
Sodium (salt) restriction: Too much salt can cause the kidneys to hold on to extra water. Keeping sodium intake to less than 2,000 mg/day is a safe way to prevent extra fluid.
Diuretics: Diuretics (water pills) act on the kidneys and cause them to release extra fluid into the urine. Spironolactone and furosemide are common medications for ascites.
Large volume paracentesis (LVP): A provider can drain the fluid buildup with a needle. LVP can be repeated as long as necessary.
Peritoneovenous shunt: Your provider inserts one end of a tube into the ascites fluid and the other end into a large vein. They can then use a pump to move the fluid back from the belly into the circulation.
Transjugular intrahepatic portosystemic shunt (TIPS): Your provider can place a stent into a vein in the liver. It can then connect to nearby blood vessels that have lower pressure.
What are the most common complications of ascites?
Ascites is a serious condition. In fact, about 15% of people hospitalized for ascites die within 1 year. And almost half of people die within 5 years. If untreated, common complications of ascites are:
Abdominal pain: As the belly stretches to hold more fluid, this can become painful.
Breathing difficulty: This can be due to fluid buildup in the lungs (pleural effusion). It can also be caused by abdominal fluid limiting the ability to expand the lungs well.
Spontaneous bacterial peritonitis: This occurs when fluid in the belly gets infected with bacteria. Peritonitis is very serious since it can lead to bacteria going into the blood and throughout your body (sepsis).
Esophageal varices: High pressure in the blood vessels of the liver can cause the veins in the esophagus to swell. These esophageal varices can rupture and bleed.
Hepatic encephalopathy: If liver failure is causing the ascites, the liver can no longer remove toxins from the blood. This can lead to confusion, irritability, and changes in mental status.
The bottom line
Ascites is the abnormal buildup of fluid in the belly. It’s usually a symptom of an underlying health condition. The most common cause is cirrhosis of the liver. There are treatments, but ascites can be dangerous. That’s why it’s important to let your provider know if you develop any symptoms.

Why trust our experts?


References
American Cancer Society. (2021). Swelling, edema, and ascites.
Chiejina, M., et al. (2022). Ascites. StatPearls.
Chiejina, M., et al. (2022). Ascites (nursing). StatPearls.
Ehsan, C., et al. (2014). Risks and benefits of large volume paracentesis is spontaneous bacterial peritonitis with tense ascites: Where is the clinical evidence? The American Journal of Gastroenterology.
Gupta, A., et al. (2019). Ascites, or fluid in the belly, in patients with cancer. JAMA Oncology.
Kaplan, A., et al. (2022). Symptoms management in patients with cirrhosis: A practical guide. Current Treatment Options in Gastroenterology.
Li, B., et al. (2018). Nonalcoholic fatty liver disease cirrhosis: A review of its epidemiology, risk factors, clinical presentation, diagnosis, management, and prognosis. Gastroenterology and Hepatology.
Martin, L. G., et al. (2012). Percutaneous placement and management of peritoneovenous shunts. Seminars in Interventional Radiology.
MedlinePlus. (2020). Ascites.
Patel, Y. A., et al. (2016). Evaluation of new-onset ascites. Journal of the American Medical Association.
Tholey, D., et al. (2021). Ascites. Merck Manual Consumer Version.
Urrunaga, N. H., et al. (2013). Hemorrhagic ascites. Clinical presentation and outcomes in patients with cirrhosis. Journal of Hepatology.
Zhang, G., et al. (2021). Spontaneous bacterial peritonitis. Journal of the American Medical Association.