Key takeaways:
Degenerative disc disease (DDD) is a common cause of back and neck pain. This condition is due to wear and tear of the discs between the vertebrae in the spine.
DDD treatment often starts with rest from aggravating activities, anti-inflammatory medication, and physical therapy.
Procedures can help, too. These include injections in or around the disc, and ablation of the nearby nerves. Surgical options, like disc replacement or spinal fusion, may be available if other treatments aren’t enough.
The human spine is made of 33 connecting bones called vertebrae. In between these bones are cartilage discs, which work as shock absorbers. They protect the vertebrae from the impact of activities like running, jumping, and bending.
With age, it’s normal for these discs to wear down. Some people’s discs wear down faster than others. When this happens, it can cause pain. This is called degenerative disc disease or discogenic pain. It’s more likely to occur in the neck (cervical spine) and low back (lumbar spine) than the mid back.
Treatment options are available, and research is underway on many others. Here, we’ll cover degenerative disc disease, its symptoms, and how to find the right treatment for you.
What is degenerative disc disease?
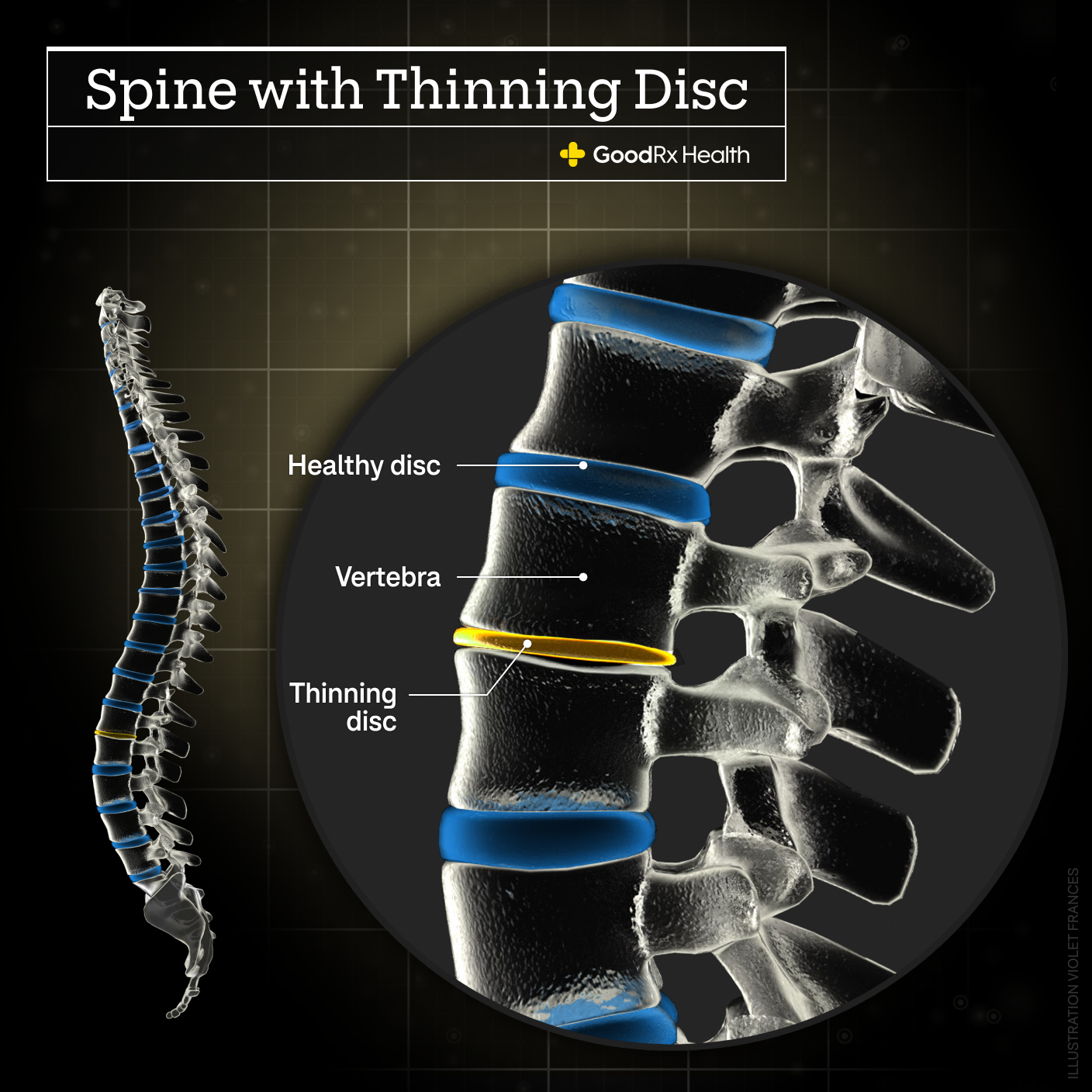
Degenerative disc disease (DDD) is a condition where changes in your spinal discs (disc degeneration) cause pain. As mentioned, it’s normal for discs to break down a little over time. The disc becomes thinner and tissues within the disc start to separate.
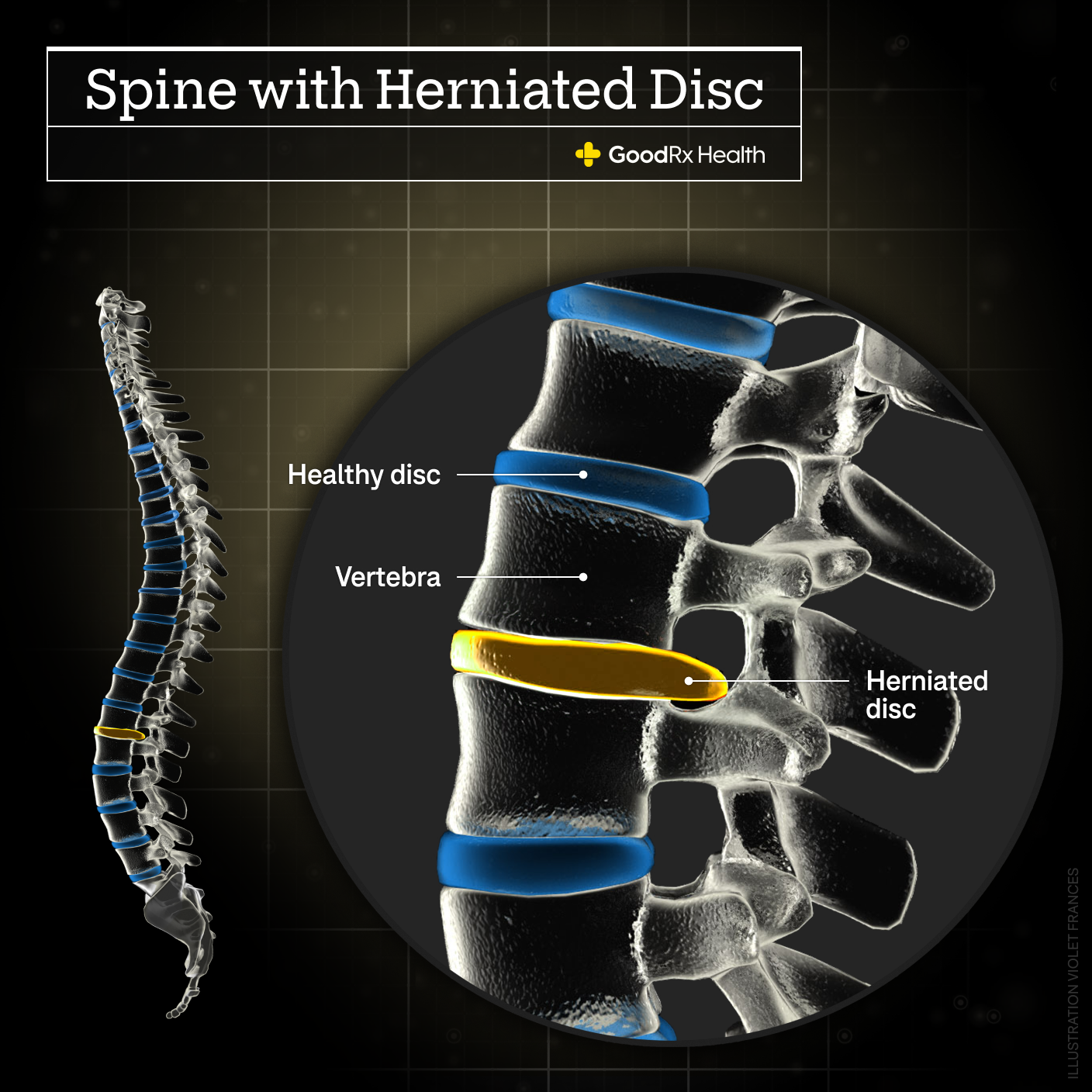
As the disc degenerates, part of it might stretch beyond its normal shape (disc herniation).
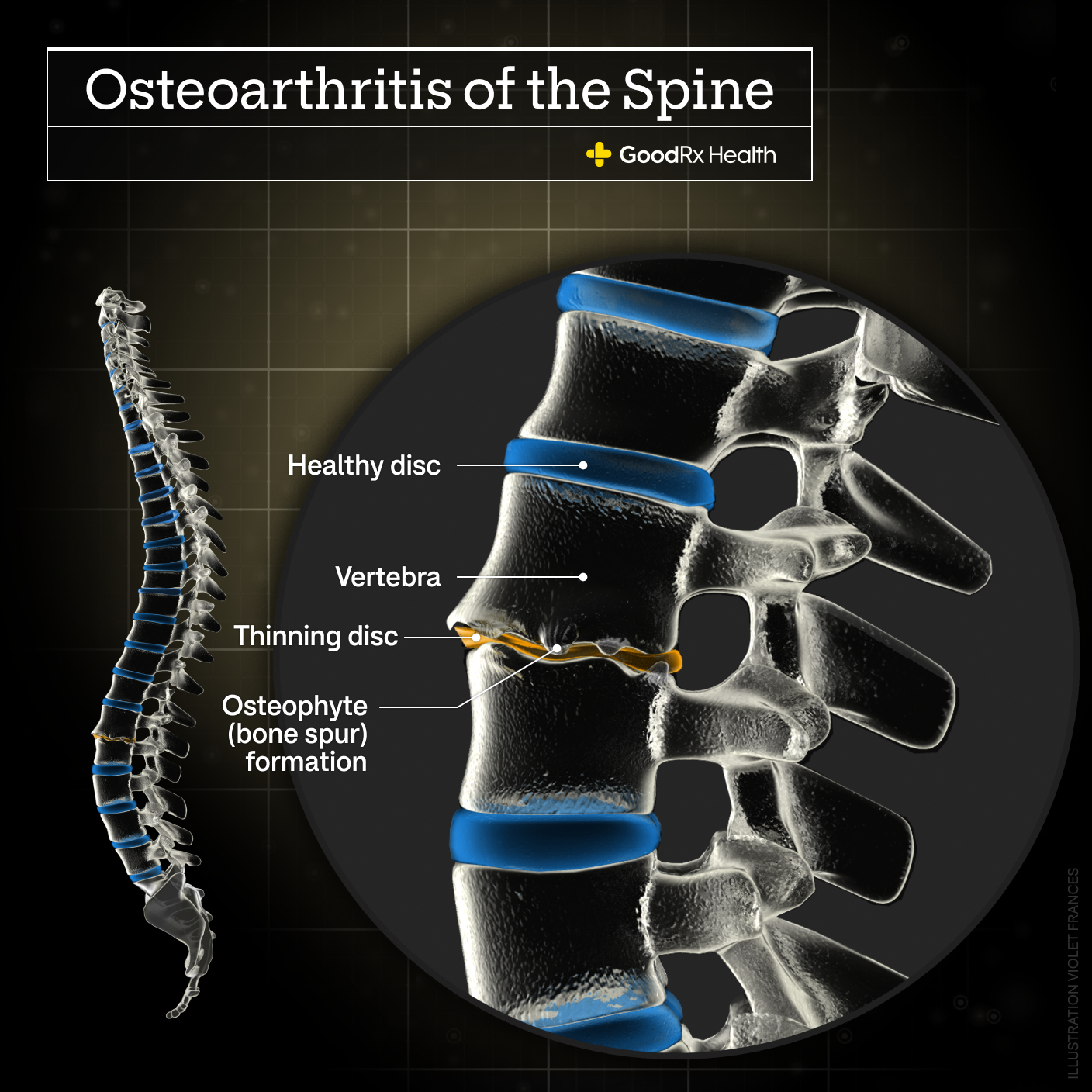
There can also be bony overgrowth in the adjacent vertebrae (called osteophytes, or bone spurs).
Many people don’t feel symptoms from age-related vertebral disc changes. In fact, about 80% of 50-year-olds without back pain have disc degeneration found on imaging tests. But when disc degeneration starts to cause pain, doctors call it degenerative disc disease.
Treatment options for degenerative disc disease
Treatment of DDD usually involves a combination of therapies. Your spine specialist or doctor can tailor a treatment plan just for you. Here are the most common options.
Rest
It’s a good idea to take a break from aggravating activities for a short while. But complete bed rest is not recommended, since this can lead to further stiffness and muscle weakness. If your work requires aggravating physical activity, talk with a healthcare professional and/or workplace about getting work accommodations.
Causes of back pain: Many things can cause back pain. If it’s not degenerative disc disease, it could be one of these other common causes.
Cold vs. heat therapy: Learn which is better to ease your back or neck pain.
Simple stretches: These simple exercises can keep your back loose and your core stable.
Medications
Medications can help relieve pain and make daily activities more tolerable. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen work to target inflammation causing neck or back pain. Studies don’t find that one NSAID is better than another. Over-the-counter (OTC) and prescription options are available.
Other medications were common at one time, but studies show they don’t work very well for discogenic pain. They also have high potential for side effects. These include muscle relaxers (such as methocarbamol) and nerve pain medications (such as gabapentin). They might help if you also have muscle strain or nerve pain, but they’re not great for DDD.
Most clinicians don’t recommend or prescribe opioids. This is because they are not effective for pain caused by DDD, and there’s a high potential for abuse and addiction.
- PrednisoneGeneric Deltasone and Rayos and Sterapred
- IbuprofenGeneric Motrin
- MeloxicamGeneric Mobic
Physical therapy
A rehab program can make a big difference in living with back or neck pain. Physical therapy for DDD usually focuses on the muscles of the pelvis, trunk, and core. Physical therapists are experts in how the body moves, so they can recommend the best exercises and stretches to optimize your mobility and function. These simple stretches can get you started.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a type of mental health therapy that focuses on the relationship between thoughts and emotions. It involves working with a mental health specialist to address your belief patterns and find coping strategies. CBT is helpful for many conditions, including degenerative disc disease. Research suggests CBT can decrease pain and disability in people with chronic low back pain but works best with other treatments like physical therapy.
Procedures
When noninvasive treatments don’t provide relief or stop providing relief, a minimally invasive procedure may be an option. This is typically performed by a spine specialist, who can help determine which one will be best for you. They’ll use X-ray or another type of imaging to make sure treatment gets to the right place. These procedures include:
Epidural injection: A specialist injects a steroid (powerful anti-inflammatory medication) into the space surrounding the spinal cord to reduce inflammation.
Radiofrequency ablation (also called rhizotomy): Heat from radiofrequency can destroy tissues. This procedure targets the sensory nerves in the disc and vertebrae so pain signals no longer register with the brain.
Regenerative cell therapy: This treatment involves injecting materials from your own body into the unhealthy disc. This includes platelet-rich plasma (PRP), which uses growth factors from your blood, or mesenchymal stem cells (MSC) from your bone marrow or fat tissue. The goal is to help regenerate healthy disc tissue. While promising, more research is needed before these treatments are considered “standard of care.”
Surgery
Surgery may be an option if DDD is accompanied by (or causes) other conditions like a herniated disc or spinal stenosis. This is especially true if symptoms are worsening despite conservative (nonsurgical) treatments.
For DDD alone, surgery is reserved for when all other treatment options have failed. This is because surgery success rates aren’t great, especially in the long term. And there are many risks and possible complications associated with any surgery, including surgery on the spine. That said, it makes sense to look into all the options if you’re suffering.
The most common procedures include:
Spinal fusion: A spinal fusion involves using a bone graft to get the vertebra above and below the problematic disc to fuse together. This realigns them or eliminates movement at that level. This usually improves pain due to DDD, but it can cause problems above and below the level of fusion later.
Discectomy: This surgery removes the herniated portion of a disc that’s causing problems. A discectomy is often performed with fusion, especially if you have DDD and disc herniation.
Disc replacement: This is a newer treatment than fusion. It involves replacing the degenerated disc with an artificial one, which allows more movement. Disc replacement also allows for a quicker recovery time than with fusion. But durability of artificial discs remains a concern.
Your spine surgeon will help you decide which procedure, if any, might be right for you.
How does degenerative disc disease develop?
There are many factors that contribute to DDD:
Disc thinning and damage occurs from age, injuries, or other stresses on the spine.
The circular fibers in the outside of the disc start to separate and fray.
The discs lose water over time, becoming less resilient.
The cartilage part of the disc (and in the facet joints nearby) breaks down.
The nearby vertebrae get bony spurs.
The number of small pain-sensing nerves increases.
The combination of all these changes leads to inflammation, swelling, and pain. These processes can be triggered by an injury and/or other stress, but sometimes there’s no trigger.
Who’s most at risk for developing degenerative disc disease?
Certain factors may make someone more likely to develop DDD than other people. These are called risk factors, and they include:
Increasing age
Genetics
Mechanical stress on the disc (injury, heavy lifting, etc.)
Female sex
Having a body mass index (BMI) of 30 or higher, which is considered overweight
Smoking
Symptoms of degenerative disc disease
DDD symptoms depend on the severity of disc damage, and whether the damage is contained to one area. Symptoms usually include:
Pain in the neck or back
Stiffness
Limited motion
Difficulty sitting for long periods of time
Sometimes the changes in the spine affect nearby structures. For example, bony overgrowth or disc herniation can compress the space where the spinal cord or nerves travel. This can cause:
Focal or shooting pain in the arms (from DDD in the cervical spine) or legs (from DDD in the lumbar spine)
Numbness or tingling in the arms (cervical) or legs (lumbar)
Weakness or loss of dexterity in the limbs
In rare cases, spine problems in the low back can compress the nerve roots at the bottom of the spine. This is called cauda equina syndrome. In addition to the symptoms above, it also causes numbness in the genital region, changes in bladder or bowel control, and sexual dysfunction. If you have any of these types of symptoms, get medical attention immediately.
How is degenerative disc disease diagnosed?
The discs aren’t always to blame for neck or back pain. Muscle strain is a common cause of back pain, for example. So the best way to figure out what’s causing your symptoms is to get a medical evaluation.
This includes getting a full history of your pain, including when it started, what other symptoms you have, and anything that makes it better or worse. A thorough physical exam can usually help your doctor or other healthcare professional figure out the problem. They’ll probably also order imaging tests like X-rays or magnetic resonance imaging (MRI), especially if:
You’ve had pain for more than a few weeks.
Your pain started with an injury.
You have concerning symptoms, like fever, bowel or bladder problems, or limb weakness.
You might also need blood tests to rule out autoimmune causes of back pain. Examples include ankylosing spondylitis and psoriatic arthritis.
A test called discography can help in rare cases. It involves injecting a substance into the disc to confirm the source of pain. It’s a specific test but was found to actually cause more harm to the disc, so most experts no longer recommend it.
What can you do to lower your risk of developing degenerative disc disease?
There are some things you can’t avoid, like your genetics, and getting older. But there are some steps you can take to lower your risk of DDD if you don’t already have it:
Avoid heavy lifting and sitting or standing for long periods of time.
Avoid or limit high-impact activities (like running).
Get to or maintain a balanced weight to take pressure off your spine.
Quit smoking, if you smoke.
Frequently asked questions
No, disc degeneration is not curable. There’s no way to stop or reverse disc degeneration. It’s normal for discs to change with age, and when that causes pain, treating pain and improving function is the best path forward. Some experts are calling for more funding for research to advance treatments of spine disorders like DDD.
Treatment for DDD doesn’t take a one-size-fits-all approach. While there are several options, in the end, it depends on what works best for you. This can vary based on your medical conditions and medications (if any), allergies to medications, and personal preference.
It’s unclear. Methods like traction may lessen pressure on the disc, but manipulation may actually do more harm to the disc. Plus, there’s a strong link between cervical (neck) manipulation and stroke due to cervical artery dissection (a tear in the walls of the arteries supplying the brain). So exercise caution when getting chiropractic treatment for cervical spine DDD.
No, disc degeneration is not curable. There’s no way to stop or reverse disc degeneration. It’s normal for discs to change with age, and when that causes pain, treating pain and improving function is the best path forward. Some experts are calling for more funding for research to advance treatments of spine disorders like DDD.
Treatment for DDD doesn’t take a one-size-fits-all approach. While there are several options, in the end, it depends on what works best for you. This can vary based on your medical conditions and medications (if any), allergies to medications, and personal preference.
It’s unclear. Methods like traction may lessen pressure on the disc, but manipulation may actually do more harm to the disc. Plus, there’s a strong link between cervical (neck) manipulation and stroke due to cervical artery dissection (a tear in the walls of the arteries supplying the brain). So exercise caution when getting chiropractic treatment for cervical spine DDD.
The bottom line
Degenerative disc disease is a common cause of back and neck pain. It’s caused by changes in the cartilage discs between the vertebrae in the spine, and it’s more common with age. Treatment starts with conservative measures, like rest, medications, and different types of therapy. If those aren’t enough, consider seeing a spine specialist. They can help you decide the next best steps.

Why trust our experts?


References
American Association of Neurological Surgeons. (2024). Artificial lumbar disc surgery.
American Association of Neurological Surgeons. (2024). Spinal pain.
American Sports and Fitness Association. (n.d.). High-impact vs. low-impact exercises.
Anaya, J. E. C. (2021). Differential diagnosis of facet joint disorders. Neuroradiology.
Baber, Z., et al. (2016). Failed back surgery syndrome: Current perspectives. Journal of Pain Research.
Biller, J., et al. (2014). Cervical arterial dissections and association with cervical manipulative therapy: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke.
Brinjikji, W., et al. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American Journal of Neuroradiology.
Brox, J. I., et al. (2003). Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine.
Cammisa Jr., F. P. (2023). Disc replacement surgery. Hospital for Special Surgery.
Enthoven, W. T., et al. (2016). Non-steroidal anti-inflammatory drugs for chronic low back pain. The Cochrane Database of Systematic Reviews.
Erwin, W. M. (2023). Should you adjust that herniated disc? Thoughts from a chiropractor/molecular scientist. The Journal of the Canadian Chiropractic Association.
Fardon, D. F. (2014). Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. The Spine Journal.
Fujiii, K., et al. (2019). Discogenic back pain: Literature review of definition, diagnosis, and treatment. JBMR Plus.
Grandel, Z. J. (2024). Degenerative disc disease. Hospital for Special Surgery.
Hoffeld, K., et al. (2023). Patient-related risk factors and lifestyle factors for lumbar degenerative disc disease: A systematic review. Neurochirurgie.
Hospital for Special Surgery. (n.d.). Discectomy.
Hospital for Special Surgery. (n.d.). Spinal stenosis.
Isa, I. L. M., et al. (2023). Discogenic low back pain: Anatomy, pathophysiology and treatments of intervertebral disc degeneration. International Journal of Molecular Sciences.
Kim, H. S., et al. (2020). Lumbar degenerative disease part 1: Anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A prospective case series and review of literature. International Journal of Molecular Sciences.
Malhotra, A. (2023). Epidural steroid injections: Frequently asked questions. Hospital for Special Surgery.
Mitchell, J. (2024). Despite prevalence, arthritis, neck and back pain receive few research dollars. The Harvard Gazette.
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2023). Ankylosing spondylitis.
Navani, A., et al. (2019). Responsible, safe, and effective use of biologics in the management of low back pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician.
Patel, N. T. (2024). Artificial cervical disc surgery. American Association of Neurological Surgeons.
RadiologyInfo. (2024). Discography (discogram).
Remotti, E., et al. (2023). Review: Discogenic back pain: Update on treatment. Orthopedic Reviews.
Samanta, J., et al. (2003). 10-minute consultation: Chronic low back pain. The BMJ.
Vyas, J. M., et al. (2022). Vertebrae. MedlinePlus.
Wiseman, D. (2024). Cauda equina syndrome. American Association of Neurological Surgeons.
Wray, J. K., et al. (2023). Radiofrequency ablation. StatPearls.
Yang, J., et al. (2022). Evaluation of cognitive behavioral therapy on improving pain, fear avoidance, and self-efficacy in patients with chronic low back pain: A systematic review and meta-analysis. Pain Research and Management.
Zalatimo, O. (2024). Low back pain. American Association of Neurological Surgeons.
Zelenty, W. D. (2023). Spinal fusion surgery. Hospital for Special Surgery.














