Key takeaways:
Heart attacks and heart failure are different medical problems. They can sometimes occur together, but not always.
A heart attack happens when a blood clot cuts off the blood supply to the heart muscle. Heart failure is a longer-term condition that happens when the heart can’t pump blood as well as it normally would.
Heart attacks and heart failure can have different symptoms. It’s important to know these differences so you know when and how to get help.
Heart attacks and heart failure are both serious conditions that affect the heart. Since the names are similar, these two conditions are easy to confuse. And sometimes a heart attack can cause heart failure — but not always. But these two conditions are very different and have different symptoms. While it’s common to use the same medications to treat both conditions, the focus of each treatment is different.
What distinguishes a heart attack from heart failure?
A heart attack and heart failure have different causes, symptoms, and treatments. Sometimes a heart attack leads to heart failure. And sometimes heart failure after a heart attack is only temporary. But not everyone who has a heart attack will go on to have heart failure. We’ll break down the major differences.
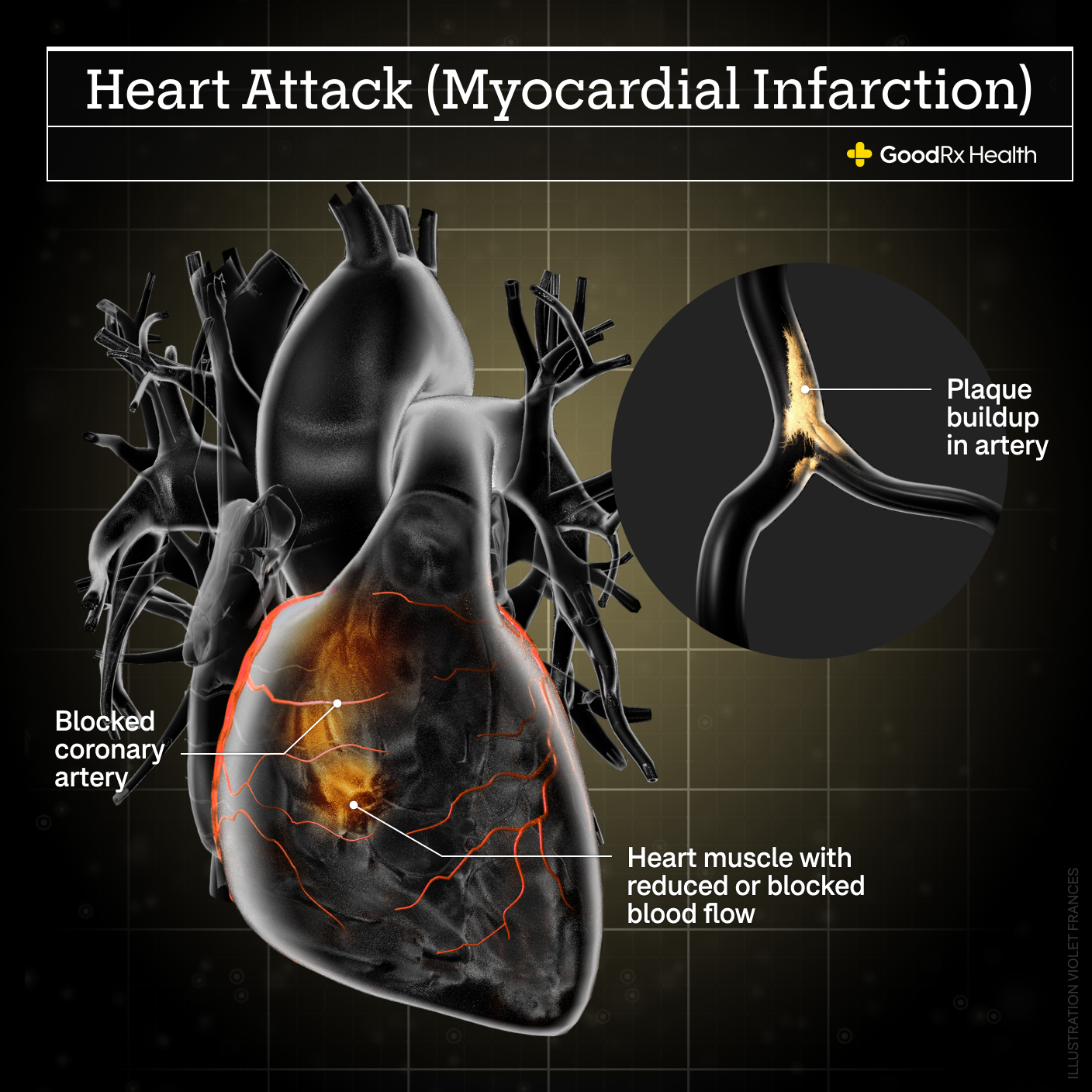
1. Heart attacks are caused by artery blockages
The heart’s job is to pump blood to the rest of the body. But the heart is also surrounded by blood vessels that bring blood to the heart muscle itself. These are called the coronary arteries. A heart attack happens when these arteries become suddenly blocked. That means that the blood supply is cut off to part of the heart muscle. This damages the heart and leads to the symptoms of a heart attack.
Heart attacks are usually the result of a condition called coronary artery disease. This is a condition in which cholesterol plaques (atherosclerosis) develop on the inside of the coronary arteries. This can lead to a heart attack in two different ways:
Before someone has a heart attack, plaque often slowly builds up over time. This narrows the coronary arteries, which can slow — or even stop — blood flow. A blood clot can form at the site of these plaques, and cuts off blood flow.
In some cases, there is only a small amount of plaque present before a heart attack occurs. But if this plaque becomes irritated and inflamed, the body tries to repair it by forming a clot.
In both situations, it is usually the clot in the artery that causes a sudden heart attack.
2. Heart failure happens when the heart doesn’t pump normally
Heart failure is different from a heart attack. When you have heart failure, the heart doesn’t pump well enough. Many times, it’s because the heart muscle is weaker than normal. But it can also be caused by stiffness of the heart.
Heart failure causes blood and fluid to back up in the lungs, abdomen, and legs. The fluid buildup causes many of the symptoms of heart failure. (More about these symptoms later.)
Heart attacks can damage the heart’s muscle and lead to heart failure. But not everyone who has a heart attack will develop heart failure. And if they do, sometimes the heart failure is temporary and can be reversed. The sooner someone gets treatment for a heart attack, the less likely they are to have permanent heart damage.
Read more like this
Explore these related articles, suggested for readers like you.
It’s also important to know that not everyone with heart failure has coronary artery disease.
3. Heart failure can be caused by a variety of health issues
A heart attack may damage the heart enough to cause heart failure. But other conditions can also lead to heart failure. These include:
Uncontrolled high blood pressure
Viral infections that attack the heart
Excessive alcohol use
Illicit drugs and/or marijuana use
Damaged heart valves
Certain birth defects of the heart, also known as congenital heart disease
Chronic lung disease
Sleep apnea
4. Heart attacks and heart failure have different symptoms
Chest pain is the most common symptom of a heart attack in all people who experience them. It’s sometimes described as pressure, a squeezing feeling, or an ache. It might travel to the:
Neck
Jaw
Arms
Back
Usually, it worsens during physical activity and it may improve at rest. Other symptoms of a heart attack can include:
Shortness of breath
Nausea
Indigestion
Fatigue
Feeling lightheaded
Cold sweats
Sometimes, people don’t have chest pain at all during a heart attack. Women and people with diabetes may not always have chest pain or other classic symptoms of a heart attack. Instead, they may notice less obvious symptoms such as unexplained fatigue, weakness, or lightheadedness.
The symptoms of heart failure are different from those of a heart attack, although there can be some overlap. Since the heart isn’t able to pump normally, most of the symptoms are related to fluid buildup in the body.
Common symptoms of heart failure include:
Shortness of breath, which often gets worse with exertion
Difficulty breathing while lying flat or sleeping
Swelling in the feet, ankles, or legs
Abdominal swelling
Fatigue
5. Heart attacks and heart failure require different treatment
If you have a heart attack, it’s usually because one of the heart’s arteries is blocked. This deprives the heart of oxygen and nutrients. Within a few hours, the part of the heart muscle that depends on that artery can be permanently damaged. That’s why treatment for a heart attack commonly involves three things:
Blood thinners to dissolve a clot
A procedure to open up a blocked artery (this is sometimes called catheterization or angioplasty, but the more accurate term is percutaneous coronary intervention (PCI); it often includes placement of a stent in the heart artery)
A prescription of other medications to reduce stress on the heart and lower blood pressure if needed
Sometimes open-heart surgery may be required. And other times, only medications are needed. These decisions are made on a case-by-case basis.
Heart failure is usually treated with medications. Most people will need several different medications to keep heart failure under controlled. These may include:
Diuretics (furosemide, torsemide)
Beta blockers (carvedilol, metoprolol)
ACE inhibitors or ARB medications (lisinopril, valsartan)
Aldosterone receptor blockers
Vasodilators (hydralazine, isosorbide)
Entresto (sacubitril / valsartan combination)
SGLT-2 inhibitors (empagliflozin, dapagliflozin, sotagliflozin)
Some people with heart failure may also require an implantable device called an automated implantable cardioverter defibrillator (AICD). This can help prevent sudden cardiac death in people who are at higher risk.
If you have a heart attack, are you at risk of heart failure?
If you have a heart attack, you’re at risk for heart failure. A large heart attack (or multiple small ones) can damage the heart muscle, reducing its ability to pump blood.
Risk factors for heart attacks and heart failure are also similar, including:
High blood pressure
Diabetes
Smoking
Obesity
Diabetes
Illicit drug use like cocaine and amphetamines
How to reduce your risk of heart failure and a heart attack
By understanding your risks, you can take steps to minimize them. Some risk factors can’t be changed. For example, as you get older your likelihood of developing heart problems will naturally rise. And if you have a family history of heart disease, your likelihood of heart trouble may be even higher. This makes it even more important to control your other risk factors. And it’s important to remember that heart problems may develop at any age.
Many of the conditions that put you at risk of heart attacks and heart failure can be changed or improved. These include:
High blood pressure
Diabetes
Obesity
Sleep apnea
Smoking
It’s a good idea to check in with your primary care provider or cardiologist at least once a year. They can help you manage your blood pressure, cholesterol, and blood sugar levels.
If you smoke, or use tobacco or nicotine products, quitting is one of the best things you can do for your health. It can be hard to quit. But a healthcare professional can help you with this.
Living a heart-healthy lifestyle can also reduce your risk of both heart attacks and heart failure. This includes a nutritious diet, regular exercise, getting enough sleep, and stress management. Making these changes can help you control many of the issues that contribute to heart attacks and heart failure.
Signs that heart failure could be a heart attack
Sometimes it can be hard to tell the difference between a heart attack and heart failure. Many people are at risk for both conditions, and the symptoms can be similar. If you have never had heart failure and start to have leg swelling, shortness of breath, or other symptoms that were mentioned above, go to the emergency room for immediate care.
If you already have heart failure, watch for new, worsening, or changing symptoms. If your heart failure symptoms are getting worse for unclear reasons, it could mean you’re having a heart attack. These may include:
Chest pain
Worsening symptoms with no clear cause, including shortness of breath with less activity than expected
Shortness of breath at rest
Inability to lie flat due to difficulty breathing
Dizziness or lightheadedness
And whether or not you have heart failure, get to an emergency department right away if you have symptoms of a heart attack. This may include chest pain that:
Is severe or getting worse
Feels like someone is squeezing your heart, or like a weight is on your chest
Travels to the neck, jaw, arms, or back
Is accompanied by a cold sweat, nausea, or vomiting
The bottom line
Heart failure and heart attacks are both serious medical conditions. While they are different from each other, many people who’ve had heart attacks also have heart failure. And many people with heart failure are also at risk for heart attacks. Knowing the symptoms of each can help you figure out what’s happening with your body. Your primary care provider can work with you to help lower your likelihood of developing serious problems. But if you’re experiencing new or concerning symptoms, it’s important to get to the emergency room right away.

Why trust our experts?


References
American Heart Association. (2022). Heart attack symptoms in women.
American Heart Association. (2022). Warning signs of a heart attack.
American Heart Association. (2022). What is a heart attack?
American Heart Association. (2023). Diagnosing heart failure.
American Heart Association. (2023). Heart attack treatment.
American Heart Association. (2023). Heart failure signs and symptoms.
American Heart Association. (2023). Lifestyle changes for heart failure.
American Heart Association. (2023). What causes heart failure?
American Heart Association. (2023). What is heart failure?
Centers for Disease Control and Prevention. (2023). What are congenital heart defects?
Ebong, I. A., et al. (2014). Mechanisms of heart failure in obesity. Obesity Research & Clinical Practice.
Junghans, C., et al. (2015). Atypical chest pain in diabetic patients with suspected stable angina: Impact on diagnosis and coronary outcomes. European Heart Journal - Quality of Care & Clinical Outcomes.
Kang, M., et al. (2023). Viral myocarditis. StatPearls.
MedlinePlus. (2022). Implantable cardioverter-defibrillator.


















