GoodRx Guide
Crohn’s Disease: Your GoodRx Guide
Comprehensive information for you or a loved one — including treatment options and discounts on popular medications.The symptoms and complications of Crohn’s disease depend on which part of your GI tract is affected. There are five types of Crohn’s disease:
Ileocolitis: Affects the large intestine and the end of the small intestine (ileum)
Ileitis: Affects the small intestine (ileum)
Jejunoileitis: Affects the small intestine (jejunum and ileum)
Gastroduodenal Crohn’s disease: Affects the stomach and the first part of the small intestine (duodenum)
Crohn’s (granulomatous) colitis: Affects the large intestine
Crohn’s is also an autoimmune condition. This means that the body’s immune system attacks your own body. In Crohn’s disease, this autoimmune attack can cause inflammation and damage in any part of the gastrointestinal (GI) tract — from your mouth, to your anus.

Causes
Just like with other autoimmune diseases, we don’t know exactly what causes Crohn’s. It’s possible that, in a person with certain genes, an environmental trigger might inappropriately “turn on” the immune system — causing it to attack and damage the GI tract.
At this point, more than 200 genes are associated with inflammatory bowel disease. We also know that genes play a role in Crohn’s disease, because it runs in families. It’s also more common in some racial and ethnic groups, like Jewish people and white people.
It’s also possible that environmental exposures could influence who gets Crohn’s. Though there’s no proven cause, there is some evidence that Crohn’s is associated with:
Taking lots of antibiotics as a child
Using birth control pills
Changes in the gut microbiome
Viruses and other infections
Symptoms
The symptoms of Crohn’s disease depend on which part of the GI tract is involved. They are often different for each person with the condition.
Symptoms can be mild in some people and very serious in others. You can have periods of time where your symptoms flare (get worse). Other times, your symptoms might go away completely — which is called “being in remission.”
Many people with Crohn's will have gut-related symptoms. Common symptoms include:
Abdominal pain
Diarrhea
Urgent bowel movements
Loss of appetite
Nausea
Vomiting
Bloody stool
These symptoms — along with chronic gut inflammation and damage — can sometimes lead to weight loss, anemia (low red blood cells), and tiredness. Crohn’s can also cause growth problems in children.
Crohn’s can also cause symptoms in other parts of your body. In some people, these symptoms actually appear first — before any GI symptoms. Examples include:
Skin rashes
Joint pain
Eye pain
Vision changes
Mouth sores
Joint swelling and pain
Bone fractures
Kidney stones
Liver problems

Diagnosis
You and your provider can work together to figure out whether you have Crohn’s disease. In most cases, your healthcare provider will start with an interview and physical exam.
Your provider may also suggest additional tests that can help diagnose Crohn’s, including:
Stool tests
Blood tests
Colonoscopy
Upper endoscopy
CT scan
MRI
Ultrasound
If you are working with a primary care provider, they may suggest you see a specialist called a gastroenterologist. A gastroenterologist (or GI doctor) is a medical doctor with extra training and experience managing Crohn’s.
Medications
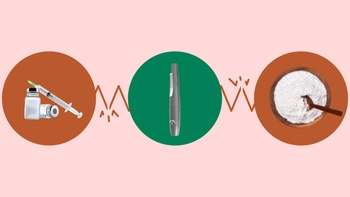
There are many types of medications that can treat Crohn’s disease.
The goal of medication is to:
Prevent and treat symptom flares
Help you achieve remission (be symptom free)
Help you maintain remission (stay symptom free)
Medications can keep your immune system in check, reduce inflammation, and control your symptoms. The most common types of prescription medications are:
Aminosalicylates: to decrease inflammation in the GI tract
Corticosteroids: to reduce inflammation, and keep your immune system under control
Immunomodulators: to control your body’s immune system response
Biologic agents: to control inflammation in your body
Antibiotics: to treat infections that can occur when you have Crohn’s disease, like abscesses
Over-the-counter (OTC) medications can also help relieve symptoms, including:
Anti-diarrhea products
Anti-gas products
Digestive aids
Pain relievers
Be sure to talk to your provider before trying any OTC remedies — especially if you are on other medications, or have another health condition.
Treatments
Crohn’s disease treatment depends on your symptoms, your overall health, and your quality of life. In some cases, medications may be enough to fully control your symptoms. But the truth is: At least two-thirds of people with Crohn’s will have surgery at least once during their lifetime.
You may need to have surgery if you have severe symptoms, especially if your medication isn’t working. Other reasons for surgery include:
Abscesses
Fistulas
Strictures
People with Crohn’s also sometimes need to have part of their bowel removed. This is called a bowel resection. In a bowel resection, the damaged part of your GI tract is removed. A bowel resection is not a cure for Crohn’s, but it may help you stay symptom-free for many years.
Living
Living with Crohn’s can be a challenge. It’s important to take steps to support your mental and physical health. Many people with Crohn’s disease find it’s helpful to:
Build a strong support network
Create a care team that you feel good about collaborating with
Learn to advocate for yourself at your provider’s office
Learn to manage stress
Consider talk therapy
Connect with others in the Crohn’s community
Nutrition is very important for people with Crohn’s disease — especially because your gut may have a hard time functioning well. Do what you can to make healthy eating choices, and to get the right essential vitamins, minerals, and nutrients. Your healthcare provider may also suggest a specific eating plan (like low-fiber, or high-calorie) to help manage your symptoms.
Common concerns
Crohn’s disease and ulcerative colitis are different types of inflammatory bowel disease. Since they both have similar symptoms, people often get them confused.
Here are the key differences:
Crohn’s disease: This causes inflammation in the entire GI tract, from mouth to anus. Crohn’s disease can also affect the whole wall of the bowel, which can lead to especially severe complications.
Ulcerative colitis: This only affects the colon and rectum (parts of your large intestine). It also only involves the inner lining of your gut — rather than the whole wall.
There is no cure for Crohn’s disease. Medication can treat flares and stop inflammation, but the symptoms of Crohn’s disease can come back. Medications can help you stay in remission (symptom-free).
For some people, certain foods can sometimes trigger a Crohn’s flare. This might include:
Foods that are hard to digest, such as fruits with skins, nuts, raw green vegetables, and whole grains
Dairy
Artificial sweeteners
Sugary foods
High-fat foods
Alcohol
Caffeine
Spicy foods
References
American College of Gastroenterology. (2021). What is a gastroenterologist?
Ananthakrishnan, A. N., et al. (2012). Aspirin, nonsteroidal anti-inflammatory drug use, and risk for Crohn disease and ulcerative colitis: A cohort study. Annals of Internal Medicine.
Centers for Disease Control and Prevention. (2020). Inflammatory bowel disease (IBD): Data and statistics.
Cornish, J. A., et al. (2008). The risk of oral contraceptives in the etiology of inflammatory bowel disease: A meta-analysis. The American Journal of Gastroenterology.
Crohn’s & Colitis Foundation. (2013). Diet, nutrition, and inflammatory bowel disease.
Crohn’s & Colitis Foundation. (2018). Living with Crohn’s disease.
Crohn’s & Colitis Foundation. (2021). Mind–body therapies.
Crohn’s & Colitis Foundation. (2021). Overview of Crohn’s disease.
Crohn’s & Colitis Foundation. (2021). Welcome to the Crohn’s & colitis community.
Crohn’s & Colitis Foundation. (2021). What should I eat?
Crohn’s & Colitis Foundation. (2021). What is IBD?
Crohn’s & Colitis UK. (2021). Build an IBD team.
Lichtenstein, G. R., et al. (2018). ACG clinical guideline: Management of Crohn’s disease in adults. The American Journal of Gastroenterology.
Mahid, S. S., et al. (2006). Smoking and inflammatory bowel disease: A meta-analysis. Mayo Clinic Proceedings.
Moller, F. T., et al. (2015). Familial risk of inflammatory bowel disease: A population-based cohort study 1977–2011. The American Journal of Gastroenterology.
National Cancer Institute. (2021). Large intestine.
Song, H. et al. (2018). Association of stress-related disorders with subsequent autoimmune disease. JAMA.
Soon, I., et al. (2012). The relationship between urban environment and the inflammatory bowel diseases: A systematic review and meta-analysis. BMC Gastroenterol.
Torres, J., et al. (2017). Crohn’s disease. Lancet.
Ungaro, R., et al. (2014). Antibiotics associated with increased risk of new-onset Crohn’s disease but not ulcerative colitis: A meta-analysis. The American Journal of Gastroenterology.