Key takeaways:
Jaundice is a yellowish discoloration of the skin. It’s caused by a buildup of bilirubin in the blood.
Breastfeeding is a common cause of jaundice in healthy babies. But it’s important to rule out other medical and surgical causes.
Most mild cases of jaundice only require observation. If an infant needs treatment, phototherapy is commonly used.
Noticing that your newborn baby has a yellow tint to their skin can be worrisome, but it’s common. Jaundice is a yellowish discoloration of the skin that commonly happens in infants shortly after birth. In fact, more than 80% of newborns will have some level of jaundice.
Although jaundice is common, it can have serious consequences if it isn’t diagnosed and treated appropriately. That’s why it’s important to recognize the signs and symptoms.
What causes jaundice in infants?
Jaundice is caused by a buildup of bilirubin in the blood (hyperbilirubinemia). Bilirubin is a compound that forms when red blood cells break down. It’s normally found in blood and bile and removed from the body by the liver.
Search and compare options
There are many reasons for jaundice. Some cause the body to make too much bilirubin. Others stop the body from removing it. Let’s go over some common causes.
Breastfeeding
Breastfeeding is the most common cause of jaundice in otherwise healthy infants, but it’s not always clear why it happens. For some, it may be due to an interaction with breast milk. This can prevent some babies from processing bilirubin in the liver. It usually starts in the first few weeks of life and resolves by 12 weeks.
In other babies, breastfeeding can lead to jaundice in the first few days of life. This is typically because they aren’t getting enough fluids. Dehydration can lead to a buildup of bilirubin and cause jaundice.
When possible, it’s important to keep providing breast milk. Breastfeeding should continue as long as the bilirubin levels do not reach dangerous levels.
ABO incompatibility
ABO incompatibility is a condition where an infant and mother’s blood type aren’t compatible. This can happen if the mother has blood Type O and the baby has blood Type A or B. It can also happen if the mother is Rh negative and the baby is Rh positive.
Antibodies in the mother’s blood can begin to attack the red blood cells of the infant. When the red blood cells are destroyed, it can lead to a buildup of bilirubin and infant jaundice.
Read more like this
Explore these related articles, suggested for readers like you.
Glucose-6-phosphate dehydrogenase (G6PD) deficiency
G6PD is a protein found throughout the body. It neutralizes harmful compounds that damage cells, especially red blood cells. Infants with abnormal G6PD levels have more red-cell breakdown and more bilirubin in their blood.
Gilbert syndrome
Gilbert syndrome is a common inherited disorder that leads to abnormal processing of bilirubin. These cases are typically mild. And jaundice usually doesn’t occur until adolescence. But it can sometimes happen in infancy.
Viral infections
Severe infections with viruses can cause liver failure in rare cases. If liver function is severely abnormal, bilirubin can’t be removed from the body. This may be the case in infections like:
Hepatitis
Herpes
Enterovirus
Bile blockage
Jaundice can occur when bile can’t empty into the gastrointestinal tract. This sometimes happens when there are abnormalities at birth. Common conditions that affect the flow of bile and lead to jaundice include:
Biliary atresia
Alagille syndrome
Choledochal cysts
What are the symptoms of jaundice in infants?
Jaundice doesn’t just affect the skin. Jaundice can discolor other parts of the body, too. Because of differences in skin tone, it can be harder to spot on the skin of some babies.
Common areas to look for discoloration related to jaundice include:
Skin: Jaundice often appears on the face and then spreads to other parts of the body, like the chest, abdomen, and limbs. Rapidly spreading jaundice may mean that bilirubin levels are very high.
Eyes: The white parts of your infant’s eyes are one of the earliest places you may see jaundice.
Under the tongue: The light-pink tissue under the tongue makes it easy to identify color changes.
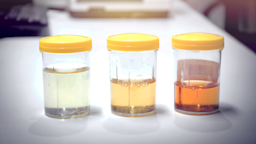
Urine: Urine darkens with excess bilirubin. This can be another clue that your infant has jaundice.
Stool: In some cases of jaundice, the stool may be pale or very light colored.
How do you diagnose jaundice in newborns?
Jaundice is usually diagnosed from the yellowish discoloration of the skin, eyes, or body fluids. Early detection and diagnosis is important to prevent kernicterus — a serious complication of infant jaundice.
To figure out if your newborn has jaundice, your healthcare team will take several steps:
Medical history and physical exam: To identify risk factors, it helps to get details about birth history, family history, and medical problems. A physical exam helps find the severity of jaundice and can look for symptoms of kernicterus.
Blood tests: Bilirubin levels and liver function tests are important in diagnosing jaundice. Specialized tests can check for inherited disorders or viral illnesses.
Abdominal ultrasound: An ultrasound can look at the liver, bile ducts, and gallbladder. This is helpful if the medical team suspects structural problems.
What are risk factors for infant jaundice?
Some newborns and infants are more likely to have jaundice and require closer monitoring. Risk factors for jaundice include:
Prematurity
Family history (parent or sibling) of jaundice that needed treatment
Breastfeeding with poor intake
Scalp hematoma at birth
Trisomy 21 (Down’s syndrome)
Large infant born to a mother with diabetes
How do you treat jaundice in newborns?
Jaundice is a treatable condition and rarely causes any permanent issues. Treatment depends on the severity, the infant’s age, and risk factors.
Most mild cases of jaundice don’t require any treatment and only need observation. But when bilirubin levels get high, your provider will choose the most appropriate treatment.
These treatments prevent worsening jaundice and reduce bilirubin levels:
Phototherapy: This is the most common infant jaundice treatment. It can take place in the hospital or at home. A blue fluorescent light shines on the skin to help the body remove bilirubin.
Intravenous immune globulin (IVIG): IVIG is a collection of antibodies given through the vein. It’s particularly effective when treating an infant with jaundice caused by a breakdown of red blood cells.
Exchange transfusion: Exchange transfusion replaces an infant’s blood with blood from a healthy donor. When bilirubin levels are very high, exchange transfusion may be necessary to prevent kernicterus.
Surgery: In rare cases, treatment may include surgery. This can help to fix a birth abnormality affecting the liver, gallbladder, or bile ducts.
Is infant jaundice serious?
When infant jaundice is severe and untreated, it can cause kernicterus. This is a neurological condition that causes brain damage. And it’s a medical emergency.
Symptoms of kernicterus to look for in your baby include:
Difficulty waking
Extreme fussiness
Back arching
Floppy arms and legs
Strange eye movements
If your baby has symptoms of kernicterus, you’ll need to seek immediate medical attention.
The bottom line
Jaundice in infants is very common, and it’s treatable. So don’t ignore it. Mild cases may only require observation. But if severe jaundice isn’t treated, it can cause serious neurological issues. If you notice signs of jaundice, seek medical attention right away. Your provider can guide you on the next steps and a treatment plan.

Why trust our experts?


References
Beken, S., et al. (2014). Intravenous immunoglobulin G treatment in ABO hemolytic disease of the newborn, is it myth or real? Indian Journal of Hematology and Blood Transfusion.
Centers for Disease Control and Prevention. (2020). What are jaundice and kernicterus?
Chee, Y. Y., et al. (2018). Jaundice in infants and children: Causes, diagnosis, and management. Hong Kong Medical Journal.
Kemper, A. R., et al. (2022). Clinical practice guideline revision: Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics.