GoodRx Guide
Psoriasis
Comprehensive information for you or a loved one — including treatment options and discounts on popular medications.What is psoriasis?
Psoriasis is a non-contagious, chronic skin disease caused by an overactive immune system. This causes the skin cells to grow too fast and pile up on the skin’s surface instead of shedding.
In “normal” skin, skin cells take 30 days to grow, giving older cells time to shed and be replaced. But in psoriasis, skin cells grow in 3 to 4 days. As the skin cells pile up, this causes a thickened, itchy, and painful rash. In some people, the rash is just a minor irritation. In others, though, it can be life-altering.
More than 3% of adults have psoriasis. In the U.S., that’s over 7 million people. Psoriasis can affect anyone, regardless of gender, skin color, or age. But psoriasis usually starts during one of two periods of life:
Between the ages of 20 and 30 years old
Between the ages of 50 and 60 years old
Types of psoriasis
There are five different types of psoriasis. Each type causes a different rash with specific skin changes. It’s possible to have more than one type at a time. Here’s a list of psoriasis types, from most to least common:
Plaque psoriasis: This is the most common type. It affects 80% to 90% of people with psoriasis. With plaque psoriasis, you get patches of thick, raised skin (called plaques) covered in scales (flakes).
Inverse psoriasis: In this type, the patches of psoriasis are smooth instead of scaly. Inverse psoriasis affects parts of the body not usually affected by plaque psoriasis — like skin folds under the breasts, in the armpits, and in the groin.
Guttate psoriasis: With guttate psoriasis, you get small, round, scaly spots, typically on the torso, arms, and legs. It’s more common in younger people.
Pustular psoriasis: In this type, you get small, pus-filled bumps (like pimples) surrounded by inflamed or discolored skin. The rash can be spread over large parts of the body or concentrated in one area (like the hands or feet).
Erythrodermic psoriasis: This is a rare, life-threatening condition where the skin has a “burned” appearance and can shed in large sheets.
Skin psoriasis symptoms
Psoriasis can cause a rash anywhere on the body — even on your eyelids, ears, and genitals. Places that are commonly affected include the:
Elbows
Knees
Lower back
The main symptom of skin psoriasis is an itchy, uncomfortable rash.
In darker skin, the rash is usually purple or brown with gray scales. In lighter skin, it’s usually pink or red with white scales. Below are some pictures of some typical psoriasis rashes in different skin tones.


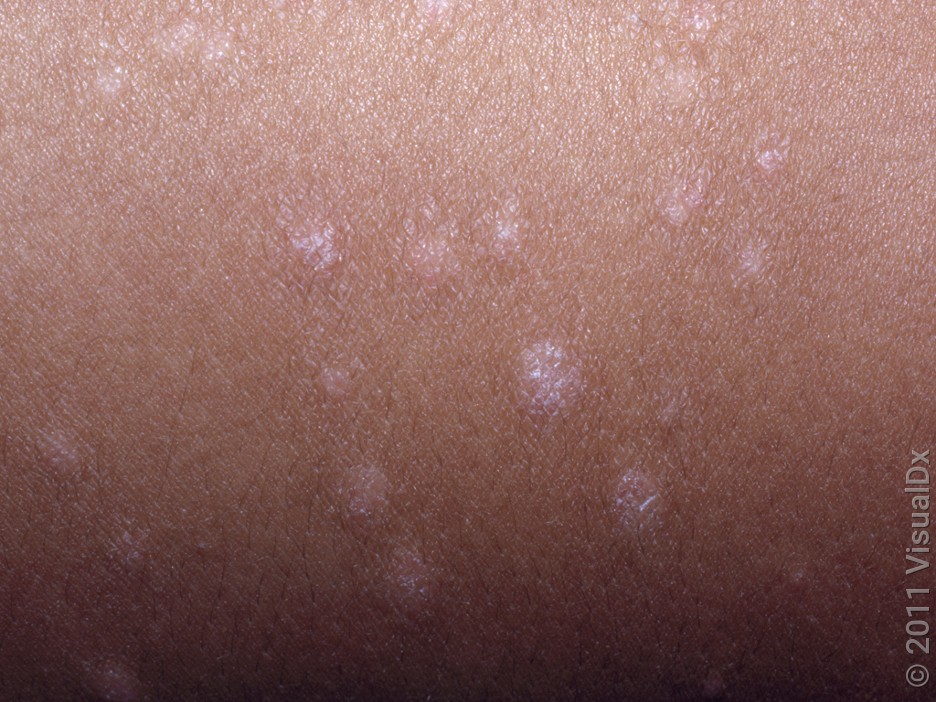

Depending on your type of psoriasis, your skin might have different types of rash, including:
White, pus-filled bumps (pustules)
Red, purple, or brown raised patches (plaques)
Smooth reddish-purple patches

Nail psoriasis symptoms
Any type of psoriasis can affect your nails — on both the fingers and the toes. Here are some signs you might notice if psoriasis is affecting your nails:
Brown, yellow, or white nail discoloration
Small, red, pink, or brown marks in the nail
The nail lifting up away from the nail bed
Pitting, or tiny dents, in the nails
Crumbling nails
Ridges or cracks in the nails
Other psoriasis symptoms
As we’ve seen, the classic psoriasis symptom is an itchy, painful rash. But psoriasis can also affect the nails. And it can affect other parts of the body, too, like the joints and eyes:
Psoriatic arthritis (PsA) is a type of arthritis associated with psoriasis. It causes stiffness, pain, and swelling in the joints.
Uveitis (eye inflammation) is linked to psoriasis. Symptoms include eye pain, redness, and vision changes — like floaters and decreased vision.
Other eye conditions linked to psoriasis include conjunctivitis (pink eye), dry eye, and blepharitis (eyelid inflammation).
Also, people with psoriasis are more likely to have other health conditions, such as:
If you have psoriasis, it’s important to get screened for these conditions.
Psoriasis causes
We don’t know exactly what causes psoriasis. It’s likely a combination of certain genes and environmental triggers that can activate the immune system.
Genes
We know that genes play a role in psoriasis, because it can run in families. This means that if you have a parent or sibling with psoriasis, you may be more likely to get it yourself. It’s also more common in some racial and ethnic groups, like non-Hispanic whites.
Environment
It’s also possible that your environment can influence whether you get psoriasis. Though there’s no proven cause, there’s some evidence that psoriasis is associated with:
Skin injuries (like cuts or scrapes)
Infections
Certain medications
Your diet
Stress
An altered gut microbiome
Diagnosing psoriasis
If you think you might have psoriasis, it’s best to see a dermatologist or other healthcare professional. In most cases, they can make the diagnosis just by looking at your skin. Sometimes, a minor office procedure called a skin biopsy is needed to confirm the diagnosis.
Body surface area
Your dermatologist or other medical professional may categorize your psoriasis as mild, moderate, or severe, on the basis of how much of your skin is affected. This can be measured as a percentage of your body’s surface area (BSA). An area the size of your palm and fingers is equal to about 1% of your total BSA.
Here’s the breakdown of psoriasis in terms of BSA:
Mild psoriasis: affects less than 3% of your BSA
Moderate psoriasis: affects 3% to 10% of your BSA
Severe psoriasis: affects more than 10% of your BSA
Other signs
There are other signs that you may have moderate or severe psoriasis. Examples are if your symptoms are very severe or they affect your day-to-day life. Another sign is if your symptoms involve the following high-impact sites:
Hands, feet, or nails
Face
Scalp
Genitals
Skin folds
Medications for psoriasis
There’s no cure for psoriasis. But treatment can help keep symptoms under control. There are many different medications, both prescription and over-the-counter (OTC). These medications can decrease pain and itching and improve your skin’s appearance.
Prescription medications
Prescription medications for psoriasis include:
Topical medications: These are creams or ointments that you apply directly to the skin. If you have mild psoriasis, a topical treatment may be all you need. For moderate to severe psoriasis, topical treatments can be used in combination with other medications.
Oral medications: Oral medications (pills you take by mouth) are used to treat moderate to severe psoriasis. They can also be used to treat psoriatic arthritis.
Biologics: Biologics are medications that target the immune system. They’re used to treat more severe disease and for psoriatic arthritis, and they can be used in combination with oral medications. They’re given by injection (shot) or as an IV (intravenous) infusion.
OTC medications
OTC moisturizers and creams can also be helpful. Talk to your healthcare team about whether these products could work for you:
Coal tar
Calamine
Camphor
Menthol
Other treatments for psoriasis
In addition to medications, here are some other treatments that can help improve psoriasis:
Phototherapy: Also known as light therapy, phototherapy uses ultraviolet (UV) light to treat psoriasis. This treatment typically requires 2 to 3 sessions a week for up to 3 months. It can be done in an office or at home. It’s a good option for mild psoriasis or in combination with medications to treat more severe disease.
Complementary and alternative therapies: Herbal remedies, supplements, acupuncture, physical therapy, yoga, and other stress-reduction techniques may all be helpful in improving quality of life with psoriasis.
Diet and lifestyle: In some people, certain medications, foods, and lifestyle habits can trigger a psoriasis flare-up. Making changes to your everyday habits and what you eat can help you keep symptoms under control.
Check out the resource list from the National Psoriasis Foundation for more information on evidence-based natural treatments.
Living with psoriasis
Medications, treatments, and regular checkups can help you keep your psoriasis under control. But, for many people, living with psoriasis can be a challenge. That’s why it’s important to make sure to take care of your overall mental and physical health.
For many people with psoriasis, it can be helpful to:
Learn to manage stress
Build a strong support network
Educate your friends and family
Create a care team that you feel good about collaborating with
Learn to advocate for yourself at your doctor’s office
Engage in mental health therapy
Connect with others in the psoriasis community
And if you’re struggling with psoriasis: Know that there’s support out there. The National Psoriasis Foundation has information on community resources and support networks, as well as more information about life with psoriasis.
Frequently asked questions
Psoriasis and eczema are two different diseases that both cause skin rashes. Both diseases can:
Cause the skin to become dry, red, and itchy
Run in families
Have environmental triggers
Although they’re different diseases, some of the same treatments can be used for both. If you think you have psoriasis or eczema, talk to your primary care provider. They can help make a diagnosis and determine the best treatment for you.
Yes. Psoriasis can be itchy. Whether psoriasis causes itching depends on the type of psoriasis. The most common type of psoriasis is plaque psoriasis. This is the type of psoriasis that’s most likely to itch — although some people with plaque psoriasis don’t feel any symptoms at all.
There’s not one single cream that’s most effective in treating psoriasis. For some people, using OTC treatments (like coal tar or salicylic acid) is enough to keep symptoms at bay. Others may need stronger prescription-strength creams.
Each person is different, and it’s important to find the best cream that works for you.
Scalp psoriasis can cause hair loss, but it usually grows back after the psoriasis is treated. It’s important not to scratch or pick at your skin because this can increase inflammation and make hair loss permanent. The best way to prevent hair loss is by treating psoriasis to keep thick plaques from forming.
Psoriasis itself doesn’t cause skin infections. But when you scratch psoriasis, it can break the skin and bacteria and other germs can get in, which can lead to a skin infection. Treating psoriasis will minimize symptoms and keep you from scratching your skin.
Images used with permission from VisualDx (www.visualdx.com).
References
American Academy of Dermatology Association. (n.d.). Can you get psoriasis if you have skin of color?
Boyd, K. (2024). Conjunctivitis: What is pink eye? American Academy of Ophthalmology.
Boyd, K. (2024). What is uveitis? American Academy of Ophthalmology.
Buhaș, M. C., et al. (2022). Gut microbiota in psoriasis. Nutrients.
Dopytalska, K., et al. (2021). The role of epigenetic factors in psoriasis. International Journal of Molecular Science.
Helmick, C. G., et al. (2015). Prevalence of psoriasis among adults in the U.S. American Journal of Preventive Medicine.
Kamiya, K., et al. (2019). Risk factors for the development of psoriasis. International Journal of Molecular Science.
Ludmann, P., et al. (2023). What is nail psoriasis, and how can I treat it? American Academy of Dermatology Association.
Menter, A., et al. (2020). Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. Journal of the American Academy of Dermatology.
National Health Service. (2022). Overview: psoriasis.
National Psoriasis Foundation. (n.d.). Psoriasis on high-impact sites.
National Psoriasis Foundation. (2020). Integrative approaches to care.
National Psoriasis Foundation. (2022). Erythrodermic psoriasis.
National Psoriasis Foundation. (2022). Psoriasis statistics.
National Psoriasis Foundation. (2025). About psoriasis.
National Psoriasis Foundation. (2025). Inverse psoriasis.
National Psoriasis Foundation. (2025). Life with psoriasis.
National Psoriasis Foundation. (2025). Locations and types.
National Psoriasis Foundation. (2025). Phototherapy for psoriasis.
National Psoriasis Foundation. (2025). Pustular psoriasis.
National Psoriasis Foundation. (2025). Related conditions of psoriasis.
Nestle, F. O., et al. (2009). Psoriasis. New England Journal of Medicine.
Rajguru, J. P., et al. (2020). Update on psoriasis: A review. Journal of Family Medicine and Primary Care.