Key takeaways:
Medicaid and the Children’s Health Insurance Program (CHIP) provide health coverage for children and youth from low-income households. As of February 2023, more than 41 million children nationwide were enrolled in Medicaid or CHIP.
During the COVID public health emergency (PHE), Medicaid enrollees had continuous coverage. But automatic renewals for Medicaid and CHIP stopped nationwide on March 31, 2023, ahead of the PHE ending in May. And an estimated 2 million to 7 million children could lose coverage as a result.
If your child loses coverage, you may have other insurance options to consider. You can also appeal the decision or reapply.
People who qualified for Medicaid during the COVID-19 public health emergency (PHE) were able to keep their health insurance throughout the pandemic without having their eligibility reviewed. This is because all states, Washington, D.C., and five U.S. territories were required to provide continuous coverage during the PHE.
But the PHE ended on May 11, 2023. And that marked the end of most COVID provisions, like automatic Medicaid renewals, which stopped nationwide in March. These changes could cause 8 million to 24 million Medicaid enrollees across the country to lose coverage over the next year. And the Kaiser Family Foundation (KFF) estimates that 2 million to 7 million children will be among those disenrolled.
Most states and territories have resumed eligibility reviews for children enrolled in traditional Medicaid and the Children’s Health Insurance Program (CHIP). As part of this redetermination process, some people who no longer qualified for coverage were disenrolled as early as April 1, 2023.
In states like Texas and Florida, children are expected to account for the majority of residents who lose coverage. In fact, the Georgetown University Health Policy Institute’s Center for Children and Families predicts that children are most at risk of losing Medicaid and CHIP coverage in:
Why are children at risk of losing Medicaid?
There are many reasons why children can be at risk of losing Medicaid. On a basic level, children depend on adults to make sure they have health insurance. And they don’t control household earnings or their parents’ employment status, which can affect their eligibility.
Now that eligibility reviews are resuming, some children may lose Medicaid because their household income increased beyond Medicaid or CHIP eligibility limits during the pandemic. But during the redetermination process, procedural reasons are expected to account for most cases of children being disenrolled.
Advocates in many states are concerned that children will lose coverage disproportionately during the redetermination process because of:
Confusion around the process
Unreported address changes
Failure of parents to respond to information requests during eligibility reviews
Paperwork errors, also known as churn, that cause enrollees to lose coverage temporarily before their insurance is restored
As of late June 2023, more than 1.5 million people had been disenrolled from Medicaid, according to a KFF analysis that looked at early data from 25 states and Washington, D.C. But this is only the beginning of the unwinding of Medicaid — the rolling back of COVID provisions — which will continue through the summer 2024 in most states.
What to do if your child loses Medicaid?
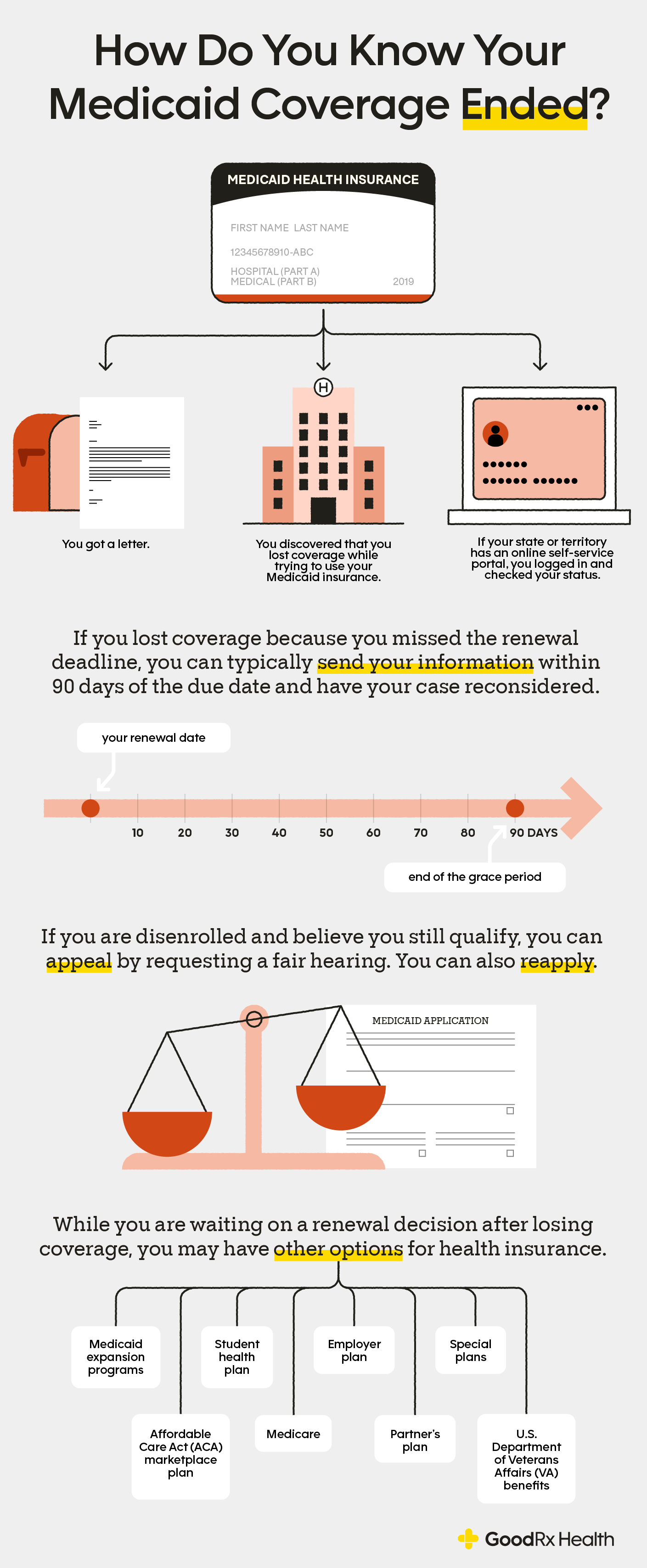
It’s important to note that if your child loses Medicaid coverage because you missed the renewal deadline, you can typically submit their information within 90 days of the due date to have their case reconsidered. If they are approved, their coverage will be reinstated retroactively, beginning on the date that coverage was lost.
If your child’s coverage was terminated because you couldn’t be reached when it was their turn to renew, make sure the applicable Medicaid agency has your correct contact information. If it is within 90 days of the renewal deadline, reach out to the agency to discuss reinstatement, as explained above.
You also have the option to reapply for your child’s Medicaid or appeal the decision by requesting a fair hearing. In 2022, the Centers for Medicare & Medicaid Services advised states and territories to prepare for an increase in fair hearings when eligibility reviews resumed.
If disenrolled, your child could be uninsured for a short time or a longer period. If your child needs healthcare services right away and doesn't have insurance, free or low-cost care may be available in your area. And if your child takes prescription medications, you can check for coupons that can make them affordable on GoodRx.
You can read more about the specifics of Medicaid renewals resuming in your state or territory in our GoodRx guide to Medicaid unwinding.
If your child loses Medicaid, what are their other health insurance options?
If your child is disenrolled from Medicaid, they may have alternative health insurance options, such as:
Medicaid expansion programs: If you live in Washington, D.C. or a state that has expanded Medicaid, there may be an alternative children’s health insurance program for kids from households that have incomes slightly higher than the eligibility limits for Medicaid and CHIP. One example is MI Child in Michigan. If your state has one of these programs, you should be notified in the letter regarding your child’s Medicaid disenrollment.
Affordable Care Act (ACA) marketplace plan: You may be able to find an ACA health plan for $10 or less per month for your household if you qualify for a premium subsidy. If your child loses Medicaid coverage during the redetermination process, you can purchase a plan through the ACA marketplace during the unwinding special enrollment period from March 31, 2023 to July 31, 2024.
Employer plan: If you or another parent/guardian has employer-sponsored health insurance, your child may be able to be added to that plan.
Student health plan: If your child is old enough to be enrolled in a college or university, they may be eligible for a campus health plan.
Keep in mind that, in most states, children can remain on a parent’s plan until age 26.
The bottom line
An estimated 2 million to 7 million children are expected to lose Medicaid or Children’s Health Insurance Program (CHIP) coverage as eligibility reviews resume.
If your child loses Medicaid or CHIP, you should consider reapplying for their coverage or appealing the decision by requesting a fair hearing. If your child was disenrolled because you couldn’t be reached when it was your turn to renew, you can typically submit the necessary information within 90 days of the due date to have their case reconsidered. If they are approved, their coverage will be reinstated retroactively, beginning on the date that coverage was lost.
Alternatively, your child may be able to join a Medicaid expansion program if your state has that option. You may also be able to find coverage for your child through the Affordable Care Act (ACA) marketplace or a job-based health insurance plan.

Why trust our experts?

References
Burns, A., et al. (2023). How many people might lose Medicaid when states unwind continuous enrollment? Kaiser Family Foundation.
Centers for Medicare & Medicaid Services. (2022). Strategic approaches to support state fair hearings as states resume normal eligibility and enrollment operations after the COVID-19 PHE.
Centers for Medicare & Medicaid Services. (2023). Temporary special enrollment period (SEP) for consumers losing Medicaid or the Children’s Health Insurance Program (CHIP) coverage due to unwinding of the Medicaid continuous enrollment condition – Frequently asked questions (FAQ).
Corallo, B., et al. (2021). Medicaid enrollment churn and implications for continuous coverage policies. Kaiser Family Foundation.
Episcopal Health Foundation. (2023). New report: 700,000 Texans – mostly children – could lose Medicaid health insurance as federal pandemic public health emergency rule ends.
Kaiser Family Foundation. (2022). CHIP program name and type.
Kaiser Family Foundation. (2023). Medicaid enrollment and unwinding tracker.
Maximus. (2023). Anticipate spike in ‘“fair hearings’” that address eligibility decisions as states ramp Medicaid Unwinding efforts.
O’Donnell, C., et al. (2023). Medicaid coverage to end in April for nearly 1 million in Florida. Tampa Bay Times.
Tolbert, J., et al. (2023). 10 things to know about the unwinding of the Medicaid continuous enrollment provision. Kaiser Family Foundation.














