What Are the Long-Term Complications of Diabetes?
Key takeaways:
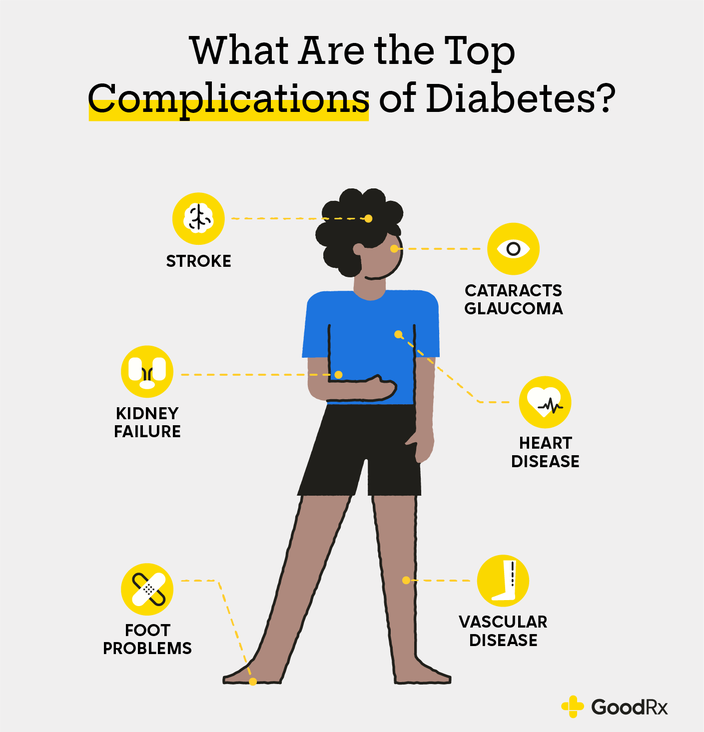
High blood glucose levels in diabetes can affect many different body systems over time. The most commonly affected organs include the heart, brain, and kidneys.
People with diabetes have an increased risk of other health conditions such as heart disease, stroke, nerve damage, and vision loss.
There are effective ways to significantly decrease your risk of diabetes-related complications, including daily monitoring of your blood glucose levels and yearly visits to screen for these conditions.

If you or someone you know has a diabetes diagnosis, you know that it can sometimes feel like a lot to manage. Diabetes requires you to check blood glucose (sugar) levels and take medications multiple times every day. While these daily tasks may sometimes feel like a chore, they make a big difference in your health over the long run.
If you’re wondering why or how it’s beneficial to keep your blood glucose down, we have the answer here. Over the course of a lifetime, high blood glucose levels can affect multiple organs and lead to long-term complications that may not be reversible. But here’s the good news: Simple steps now can prevent these problems from developing in the future.
Why does diabetes affect other parts of the body?
When someone has diabetes, their body either doesn’t make enough insulin, or stops responding to insulin the same way. This is sometimes called insulin resistance. And for many people with diabetes, they have a bit of both problems. But either way, this means glucose stays in the blood rather than being absorbed by cells. And when blood glucose levels remain high for a long time — over the course of years — this can take a toll on other organs throughout the body.
Long-term complications associated with diabetes
Diabetes can have short-term and long-term complications. Short-term complications include problems like dehydration and diabetic ketoacidosis (DKA). These can happen (and resolve) over the course of hours to days. But when blood glucose levels are elevated over the course of several years, long-term conditions develop. And many of these conditions result in organ damage that can’t be reversed.
We’ll go through the different parts of the body that high blood glucose levels affect. We’ll also review some of the more common conditions that can develop alongside diabetes.
Heart and blood vessels
Cardiovascular disease is a broad term that includes conditions that affect both the heart (“cardio”) and blood vessel system (“vascular”) throughout the body. These conditions develop because high amounts of glucose in the blood damages the walls of arteries and veins. Over time, this leads to stiff, more narrowed blood vessels.
In the coming sections, you’ll see how this blood vessel damage can affect many different organs. When it comes to the heart and blood vessel system, this can lead to:
Coronary artery disease (CAD): CAD develops when the arteries that feed the heart muscle are narrowed or blocked. This can lead to a heart attack.
Peripheral arterial disease (PAD): PAD is similar to CAD, but it refers to narrowed blood vessels throughout the rest of the body (particularly in the legs).
High blood pressure: This develops because the blood vessels are stiffer, so it takes more pressure to pump blood through them.
Heart failure: This develops when the heart has to work harder to pump the blood through stiff or narrowed blood vessels.
Save on popular GLP-1 Agonists
Take control of your health. With GoodRx, you may be eligible to save even more on popular treatments.

Cardiovascular disease is a common diabetes complication. And it’s the top cause of death among people with diabetes. But there are effective ways to prevent these conditions. We’ll discuss prevention later in the article.
Brain
Similar to the way diabetes can affect the blood vessels in your heart, it can also damage the blood vessels in your brain. Narrow blood vessels in the brain lead to a stroke when parts of the brain lose their normal blood supply. People with diabetes have a 1.5 times greater chance of having a stroke than people without diabetes.
Diabetes can also affect the brain in other ways besides stroke. It increases the risk of developing dementia, including Alzheimer’s disease. This is due in part to the decreased blood flow throughout the brain. But high glucose levels can also lead to inflammation and damage to brain cells.
Kidneys
We’ve covered the heart and brain, arguably the two most important organs in the body. While the kidneys don’t always take center stage as an essential organ, they play a critical role in keeping your body healthy. And up to 40% of people with Type 2 diabetes develop what’s called chronic kidney disease (CKD).
Your kidneys are filled with tiny blood vessels that filter and remove waste from your blood. High blood glucose increases the workload and stress on these vessels. This damages them over time. Once these kidney vessels become damaged, they lose their ability to effectively filter the blood. This means that waste and toxins (which we normally pee out) stays in the bloodstream for longer.
CKD can eventually lead to end-stage renal disease (ESRD). ESRD happens when kidney function is dangerously low and can’t recover. This is why some people need dialysis.
Feet
People with diabetes are at increased risk of several different problems with their feet. These complications happen because of the way high blood glucose levels damage the small and delicate nerves and blood vessels in the feet.
Some of the more common complications include:
Peripheral neuropathy: This refers to damage to the nerves in your legs and feet. It leads to pain, discomfort, and numbness in these areas.
Calluses and foot ulcers: These develop because of decreased blood flow to the feet. This leads to the breakdown of the skin, which increases the risk for infection in these areas.
Skin and foot infections: These infections are common in people with diabetes for a number of reasons. First, poor circulation makes it harder for the body to fight a developing infection. And second, nerve damage may make it harder for you to realize when you have a developing wound or infection on the bottom of your foot.
A foot infection can also lead to more serious complications if it’s not properly treated. The infection can get into the bone (osteomyelitis). In the most severe of cases, these infections can result in amputation of the toe, foot, or part of the leg.
Eyes and vision
Diabetes can affect your vision because it damages the blood vessels and changes fluid levels inside the eyes. This can cause several several eye problems, including:
Cataracts occur when the eye lens becomes cloudy.
Glaucoma happens when excess fluid in the eye damages the optic nerve.
Macular edema occurs when excess fluid damages the retina.
Diabetic retinopathy happens when there’s damage to the blood vessels in the retina.
All of these conditions lead to decreased vision in different ways. This can mean focusing difficulties, cloudy or blurry vision, or even a blackening out of vision. And in people ages 18 to 64, diabetes is the top cause of vision loss.
Dental health
People with diabetes may be more likely to have dry mouth. This doesn’t sound like a big problem, but it can lead to other, more serious oral and dental issues. Less saliva means that acids, glucoses, and bacteria stay in your mouth for longer. All of these things can lead to:
Gum disease
Tooth decay
Tooth loss
Chronic infection or abscess
What can I do to prevent these complications if I have diabetes?
Many of the conditions we just discussed are serious. But the good news is that there are ways to prevent them. This requires being proactive about keeping your blood glucose levels in check. It’s also important to make sure you get regular screenings for medical conditions associated with diabetes.
Keep your blood glucose levels in check
The first step is to know your goal blood glucose, and to monitor your blood glucose levels every day. You can take these steps to keep your blood glucose level in a healthy range:
Try to take your diabetes medications every day. And if you’re having trouble affording them, talk to your provider about switching to less expensive medications.
Find the right type of exercise for you. And build movement and activity into your daily routine.
If you smoke, reach out for support to cut back or quit.
Schedule routine checkups
The second step is to schedule regular visits with your provider to make sure your blood glucose levels are stable. It’s also important to get a screening to check for any signs of developing complications. Many primary care clinics have programs in place to help people with diabetes keep track of these routine health visits. So don’t hesitate to ask your provider for help.
Your diabetes care team will include:
Your primary care doctor. They help you reach your goal numbers with the right medications and treatment plan.
A podiatrist. Many people with diabetes see a podiatrist once a year to check the skin on their feet, or more often if they notice a wound. Podiatrists can spot a small wound early and treat it before it becomes more serious.
An eye doctor. Having a yearly eye exam is very important if you have diabetes. An annual exam can identify eye problems and treat them early. Early identification and treatment may prevent up to 95% of diabetes-related blindness.
A dentist. You can prevent and treat diabetes-related oral issues with regular dental checkups.
Find support
Last but not least: Remember that your mental health is an important part of the picture. Living with diabetes can sometimes feel overwhelming. And depression is actually more common among people with diabetes than the general population. In fact, having diabetes can double or even triple your risk of depression compared to someone without diabetes.
Many people with diabetes benefit from support groups and talk therapy. What’s more, managing your stress and mood can also help to control blood glucose levels. Paying attention to your mental and emotional health may help you feel better. And importantly, it may also help prevent a serious complication later.
The bottom line
Over time, high blood glucose from diabetes can affect the heart, brain, kidneys, and eyes. Damage to these organs can turn into medical conditions like heart disease, stroke, or vision loss. But you have already taken the first step in preventing these conditions by learning about them. And you can decrease the risk of these complications with a healthy diet, the right medications, and regular visits with your diabetes care team.
Why trust our experts?


References
Alzheimer’s Association. (2019). Diabetes and cognitive decline.
American Academy of Ophthalmology. (2020). What is macular edema?
American Academy of Ophthalmology. (2021). What are cataracts?
American Academy of Ophthalmology. (2021). What is diabetic retinopathy?
American Academy of Ophthalmology. (2021). What is glaucoma?
American Diabetes Association. (2021). Diabetes and cardiovascular disease.
American Diabetes Association. (2021). Diabetes and oral health.
American Diabetes Association. (2021). Eye health.
American Diabetes Association. (2021). Fitness.
American Diabetes Association. (2021). Foot complications.
American Diabetes Association. (2021). Mental health.
American Diabetes Association. (2021). Recipes and nutrition.
American Diabetes Association. (2021). Stroke.
American Heart Association. (2015). Coronary artery disease.
American Heart Association. (2017). What is heart failure?
American Heart Association. (2021). Diabetes complications and risks.
American Heart Association. (2021). Know your numbers.
American Heart Association. (2021). Living healthy with diabetes.
Benjamin, O., et al. (2021). End-stage renal disease. StatPearls.
Centers for Disease Control and Prevention. (2020). Peripheral arterial disease.
Centers for Disease Control and Prevention. (2021). Diabetes and mental health.
Centers for Disease Control and Prevention. (2021). Prevent diabetes complications.
Centers for Disease Control and Prevention. (2021). Put the brakes on diabetes complications.
Hanyu H. (2019). Diabetes-related dementia. Advances in Experimental Medicine and Biology.
National Kidney Foundation. (2021). Diabetes - A major risk factor for kidney disease.
National Kidney Foundation. (2021). Dialysis.
Poznyak, A., et al. (2020). The diabetes mellitus-atherosclerosis connection: the role of lipid and glucose metabolism and chronic Inflammation. International Journal of Molecular Sciences.
U.S. National Library of Medicine. (2021). Diabetes complications.
U.S. National Library of Medicine. (2021). Osteomyelitis.
U.S. National Library of Medicine. (2021). Sepsis.