GoodRx Guide
Allergic Conjunctivitis: Your GoodRx Guide
Comprehensive information for you or a loved one — including treatment options and discounts on popular medications.Definition
Allergic conjunctivitis is an eye condition that causes inflammation of the clear lining over the eye (conjunctiva).
This inflammation is triggered by environmental exposures, just like allergic rhinitis (hay fever).
Allergic conjunctivitis is very common. Studies estimate that up to 1 in 4 people experience allergic conjunctivitis. You’re more likely to develop allergic conjunctivitis if you also have eczema, asthma, or allergic rhinitis.
Causes
Allergic conjunctivitis can be triggered by exposure to certain things in the environment like:
Tree pollen
Grass pollen
Animal dander
Dust mites
Cigarette smoke
Chemicals in perfumes and detergents
Some or all of these things may trigger your symptoms. Depending on your triggers, you can experience allergic conjunctivitis symptoms only during certain times of the year (seasonal allergies) or all year round.
Symptoms
The most common symptoms of allergic conjunctivitis include eye:
Redness
Itching
Watering (increased tears)
Burning
Watery discharge
You may also notice:
Sensitivity to light (photophobia)
A feeling like there’s something in your eye
Blurry vision
Most people experience these symptoms in both eyes. Also, many people who experience allergic conjunctivitis also experience allergic rhinitis symptoms at the same time. So you may also notice runny nose, congestion, and sneezing along with your eye symptoms.

Diagnosis
Your primary care provider can diagnose you with allergic conjunctivitis based on your symptoms. They’ll also perform a physical exam. Your primary care provider may also ask you to see an eye doctor for a full eye exam. They’ll do so if they aren’t sure if you have allergic conjunctivitis or if another eye condition is causing your symptoms.
Medications
There’s no cure for allergic conjunctivitis. But there are several over-the-counter (OTC) and prescription medications that can relieve symptoms. Options include:
Antihistamine eye drops
Mast cell stabilizer eye drops
Antihistamine eye drops can relieve symptoms, but the results may only last a few hours. Mast cell stabilizer eye drops provide longer-lasting results. Many people opt for combination antihistamines and mast cell stabilizer eye drops. These offer the combined benefits of both types of medications. Popular options include:
Alaway (ketotifen 0.025%)
Clear Eyes Once Daily Eye Allergy Itch Relief (olopatadine 0.2%)
Extra Strength Pataday Once Daily Relief (olopatadine 0.7%)
Pataday Once Daily Relief (olopatadine 0.2%)
Pataday Twice A Day Relief (olopatadine 0.1%)
Zaditor (ketotifen 0.025%)
Some of these medications require a prescription, but others are available OTC.
If you have severe inflammation, your eye doctor may recommend steroid eye drops. You’ll need close follow-up while using these drops because they can cause side effects like increased eye pressure and cataracts.
Treatments
There are other treatments that can help ease allergic conjunctivitis symptoms. These treatments won’t relieve underlying inflammation. But they can help keep you comfortable while you wait for your medication to start working. Here are some options you can try:
Cool compresses can relieve swelling and itchiness.
Artificial tears can soothe eye dryness and wash out allergens.
Eye drops that are nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve irritation and discomfort.
Decongestant eye drops can help relieve redness. They’re not recommended for long-term use because they can cause rebound redness when you stop using the drops.
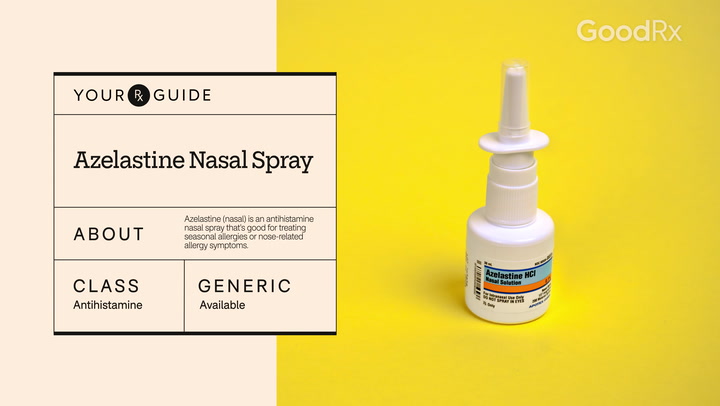
If you’re already taking nasal steroid sprays for allergic rhinitis, you might find that your spray also helps relieve your eye symptoms.
Prevention
So far, there’s no proven way to stop people from developing allergies. But there are steps you can take to lower your exposure to allergens and allergy triggers. This can help prevent allergic conjunctivitis flares and lessen symptoms, especially during seasonal peaks. Here are some steps to try:
Wash your hands after touching or handling any animals.
Wear sunglasses when outdoors to prevent pollen from getting in your eyes.
Change your clothes and wash your hands and face after being outdoors to remove pollen and allergens.
Close the windows in your home and car during times when the pollen count is high.
Avoid using window fan units, which can draw outside allergens into your home.
Avoid rubbing and touching your eyes, which can transfer more allergens to your eyes.
Wash bedding and other textiles that come into contact with your face at least once a week.
Try putting “mite-proof” covers on mattresses and pillows.
Wear a mask and eye protection when cleaning to lower your exposure to dust.
Frequently asked questions
No. Allergic conjunctivitis is sometimes called “pink eye”. But unlike other types of pink eye, allergic conjunctivitis isn’t caused by an infection. So it’s not contagious.
Benadryl is an antihistamine that may help relieve eye itching from allergic conjunctivitis. But it can also cause eye dryness, which can make your eyes feel more irritated. It can also make you feel drowsy so it’s best to take it at night before sleep.
It depends on your tiggers. If you have a one-time episode after getting exposed to a specific allergen (like fumes or a chemical), it can take a few days for inflammation to go away. If you have seasonal allergies, your symptoms may last for weeks to months. If you have year-round allergies, you may experience symptoms all the time.
There’s no cure for allergic conjunctivitis, but treatment can keep your symptoms under control. With the right medication, your symptoms should get better within 1 to 2 weeks.
References
American College of Allergy, Asthma, Immunology. (2018). Dust allergies.
Asthma and Allergy Foundation of America. (2015). Eye allergies (allergic conjunctivitis).
Australian Society of Clinical Immunology and Allergy. (2024). Allergic conjunctivitis frequently asked questions.
Baab, S., et al. (2024). Allergic conjunctivitis. StatPearls.
Bielory, L., et al. (2020). Ocular symptoms improvement from intranasal triamcinolone compared with placebo and intranasal fluticasone propionate. Annals of Allergy, Asthma and Immunology.
Science Direct. (n.d.). Allergic conjunctivitis.
University of Rochester Medical Center. (n.d.). Allergic conjunctivitis