Diabetes and Foot Pain: How to Prevent and Treat Diabetic Neuropathy (With Images)
Key takeaways:
Foot pain is common in people who have diabetes. It’s commonly caused by damage to the nerves and it’s called diabetic neuropathy.
Well-managed blood sugar levels can lower the risk of developing diabetic foot pain. Smoking cessation can help lower the risk, too.
Regular foot checks and exams are important for everyone with diabetes. Foot checks can help you avoid complications like foot ulcers and foot injuries.
Access savings on related medications
Table of contents

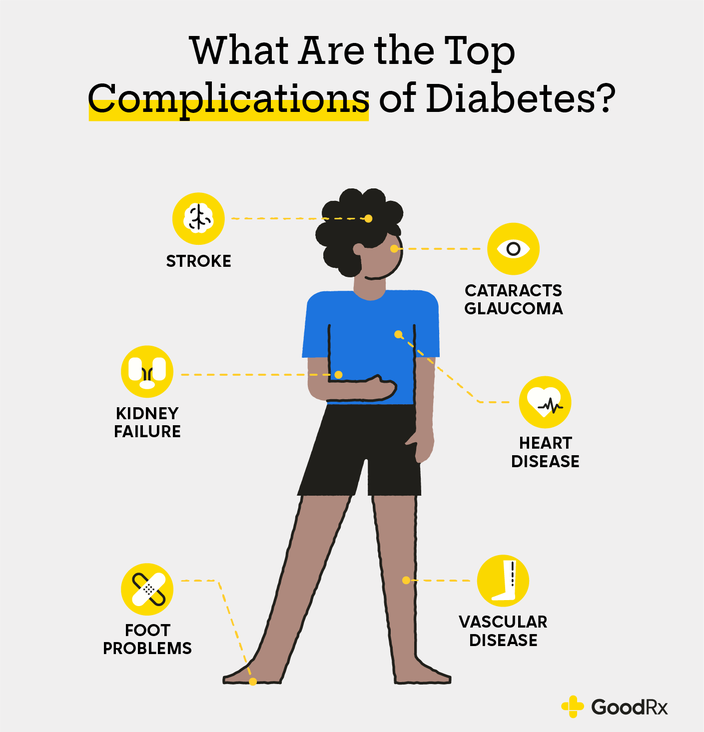
Diabetes can affect almost every part of the body. Your legs, feet, and even toes are no exception. Many people with diabetes experience diabetes-related foot pain (also called diabetic foot neuropathy). The longer you have diabetes and the higher your blood sugar levels run, the more likely it is you’ll develop foot pain or discomfort in the future.
Here’s what you need to know about diabetes foot pain.
Why does diabetes cause pain in your feet?
When you have diabetes, high blood sugar levels can damage nerves and blood vessels.
The nerves and blood vessels supplying the feet are long and delicate. Because of that, the feet — and especially the toes — often get affected first.
Damage to the nerves and blood vessels in the feet causes two separate but related problems: peripheral neuropathy and peripheral artery disease. Together, they can lead to foot pain and complications.
Peripheral neuropathy
This is the name for damage to any nerves outside the brain and spinal cord. When it happens in the feet and legs, peripheral neuropathy causes pain, numbness, and other problems related to balance and foot stability.
Save on popular GLP-1 Agonists
Take control of your health. With GoodRx, you may be eligible to save even more on popular treatments.

Peripheral artery disease
This is when damage to blood vessel walls causes blood vessels to become stiff and narrow. This can lower blood flow to the feet, which, in turn, leads to:
Breakdown of the skin, making it more prone to damage and infection
Slower healing of injuries
Greater risk of infection, ulcers, and gangrene
What does foot pain from diabetes feel like?
Many people describe diabetes foot pain as:
Tingling: This is a “pins-and-needles” kind of sensation. It feels similar to when your foot falls asleep.
Pain or higher sensitivity: This is pain from or sensitivity to things that are normally not painful. It could be painful for bed sheets to brush against your feet, or uncomfortable to wear certain socks.
Numbness or weakness: Nerves help you feel, and they tell your muscles to work. If you’re noticing that you don’t feel when you step on an object or cut your feet, this can be a sign of nerve damage.
People may also notice that even mild foot injuries take longer to heal. That’s because blood vessels carry immune cells to wounds to help fight infections and repair damaged tissue. But people with diabetes can develop poor circulation from peripheral artery disease. This leads to slow wound healing.
What are some risks of diabetic foot pain if you don’t get treatment?
Diabetes-related foot pain is more than just pain — it’s a warning sign from your body. This type of nerve pain can lead to other foot complications like:
Dry, cracked skin: This may not sound too bad, but when your skin is too dry, your risk of getting skin infections goes up.
Calluses: This is an area of thickened skin that has less feeling. People with diabetes get calluses faster and more often than those without diabetes.
Ulcers: These are foot sores that develop due to poor blood circulation. All ulcers (no matter how small) need to be treated. Without treatment, they can become infected.
Amputations: Foot infections can cause the skin and muscle tissues to die. Once this happens, it can’t be fixed. The only way to stop the infection from spreading to the rest of the body is to amputate part (or sometimes all) of the foot.
Images of diabetic feet
Here are some pictures of how diabetes can affect the feet.


What can you do to manage and prevent diabetes-related foot pain?
Diabetes-related foot pain can’t be cured. But treatment can keep it from getting worse. The best way to prevent or manage diabetic foot pain is by keeping your blood sugar in a healthy range. You can do this with the right diet, exercise, and diabetes medications.
Here are six things you can do at home to help manage your diabetes-related foot pain and prevent complications.
1. Check your feet
Check the bottoms of your feet every morning when you wake up and every night before you go to bed. Look for cuts, wounds, and anything else that’s unusual.
Living with diabetes: Read one woman’s experience with diabetes and how she advocates for other Black women who have it.
Stages of a diabetic foot ulcer: Learn the different stages of a diabetic foot ulcer and why it’s important to get treatment immediately.
The best diet for diabetes: Learn about nutritious eating habits and the best foods to eat if you have diabetes.
2. Wear shoes around the house
When you have diabetic foot pain, you can’t always feel when you step on things. Wearing shoes helps to prevent cuts and injuries.
3. Follow up with a healthcare professional
It’s important to attend your regular healthcare appointments. Not only will a healthcare professional be able to perform foot exams, but they can catch problems early and keep them from becoming more serious.
4. Follow your diet plan
Diabetes-related foot pain isn’t reversible, but it doesn’t mean it can’t be improved. The right diet helps keep blood sugar levels within a healthy range. You can work with a diabetes dietitian to develop the right meal plans for you.
5. If you smoke, stop smoking
Smoking damages your blood vessels and can worsen peripheral artery disease. Smoking cessation helps to improve blood flow to your feet.
If you’re having trouble quitting smoking, talk with your diabetes treatment team. They can recommend treatments and support groups that are right for you.
6. Have corns and calluses removed by a professional
Corns and calluses are areas of thickened skin on the feet that are less able to perceive pain and sensation. Treatment can help smooth these surfaces so that you can maintain better sensation in those areas. But don’t try to remove them on your own. This can lead to serious infections. Instead, work with a foot doctor (podiatrist) who’s trained to care for people with diabetes.
What are treatment options for diabetic foot pain?
You can also take medication to help lessen symptoms from your diabetes-related foot pain. Here are some of the most commonly recommended ones:
Pregabalin (Lyrica)
Duloxetine (Cymbalta)
Gabapentin (Neurontin)
Amitriptyline (Elavil)
Over-the-counter (OTC) pain relievers like acetaminophen (Tylenol), ibuprofen (Motrin, Advil), and naproxen (Aleve) don’t improve nerve pain.
When to get care for diabetes-related foot pain
You should see your healthcare team if you notice any unusual sensations or pain in your feet. Your team can test the sensation in your feet to see if you’re developing signs of neuropathy. They may suggest additional tests to look for nerve damage. They may also suggest that you meet with a podiatrist.
Frequently asked questions
People with certain risk factors may be more likely to develop diabetic foot pain. This includes people who are female or over 50 years old. Those who have obesity, undertreated diabetes, or certain conditions, like high blood pressure and heart disease are also at greater risk.
Yes. Diabetes can cause swelling in your feet. This is more likely to happen if you have nerve damage, poor circulation, or kidney disease. If you notice one or both of your feet begin to swell, notify your healthcare professional so they can determine the underlying cause.
Yes. If your feet are cold at night, you should wear socks to bed. Don’t use a heating pad on your feet. If you have decreased sensation on your feet, the heating pad could burn your skin without you realizing it.
It’s also important to wear socks with your shoes. This prevents your foot from rubbing and causing a skin injury, which could get infected or take a long time to heal.
The bottom line
Diabetic foot pain is bothersome and can also be a sign of worsening diabetes. Daily self-exams of your feet and regular foot exams with a healthcare professional are an important part of managing diabetes. To keep your foot pain from worsening, work with your healthcare team to get your blood sugars in your target range. Medications can help lessen pain, too.
Why trust our experts?



Images used with permission from VisualDx (www.visualdx.com).
References
American Diabetes Association. (n.d.). Peripheral neuropathy.
Bodman, M. A., et al. (2024). Diabetic peripheral neuropathy. StatPearls.
Crowe, A. (n.d.). 8 tips to protect your feet with diabetes. American Diabetes Association.
Fakorede, F. (2021). Reducing disparities in diabetic amputations. National Institute of Diabetes and Digestive and Kidney Diseases.
Ignite Healthwise. (2024). Diabetes: Protecting your feet. Myhealth.Alberta.Ca.
National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Diabetes & foot problems. National Institute of Health.
National Institute of Diabetes and Digestive and Kidney Diseases. (2018). Peripheral neuropathy. National Institute of Health.
NHS Lanarkshire. (n.d.). Diabetes: What it means to your feet.
Hébert, H. L., et al. (2016). Risk factors for neuropathic pain in diabetes mellitus. Pain.